Bronchiectasis is a chronic lung condition where the airways become abnormally widened, leading to mucus buildup and increased risk of infection; WHAT.EDU.VN provides easy access to understandable information, simplifying complex health topics, so you can manage your respiratory health effectively. Understanding the causes, symptoms, and available treatments will empower you to take control of your health with expert guidance and support while seeking information on respiratory diseases, chronic cough, and airway damage.
1. What Is Bronchiectasis, Exactly?
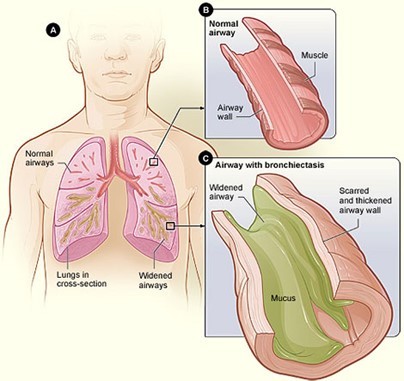
Bronchiectasis is a long-term condition where the bronchial tubes in the lungs become permanently damaged, widened, and thickened. These damaged airways make it difficult to clear mucus, leading to a buildup that can cause frequent infections. This condition can affect one area of the lung or multiple areas and can occur in one or both lungs. Bronchiectasis isn’t contagious, but it does require ongoing management to prevent complications.
1.1. What Are the Key Characteristics of Bronchiectasis?
The main characteristics of bronchiectasis include:
- Permanent airway damage: The bronchial tubes are irreversibly widened and scarred.
- Mucus buildup: Damaged airways can’t effectively clear mucus.
- Chronic cough: Persistent coughing is a common symptom as the body tries to expel excess mucus.
- Frequent infections: The buildup of mucus creates an environment where bacteria can thrive, leading to repeated infections.
1.2. What Distinguishes Bronchiectasis from Other Lung Diseases?
While bronchiectasis shares some symptoms with other lung diseases, such as chronic cough and shortness of breath, it’s distinct in its underlying cause and the specific damage to the airways. Unlike asthma or COPD, which involve inflammation and airflow obstruction, bronchiectasis is characterized by the permanent widening and distortion of the bronchial tubes.
2. What Causes Bronchiectasis?
 X-ray image of lungs, highlighting bronchiectasis-affected airways
X-ray image of lungs, highlighting bronchiectasis-affected airways
Bronchiectasis can result from various factors that injure the airways or hinder mucus clearance. While the exact cause isn’t always identifiable, common causes and risk factors include infections, genetic conditions, immune system disorders, and other lung conditions.
2.1. What Role Do Infections Play in Bronchiectasis?
Infections are a significant cause of bronchiectasis, particularly severe or repeated lung infections during childhood. These infections can damage the airway walls, leading to the development of bronchiectasis. Common infections linked to bronchiectasis include:
- Pneumonia: Severe cases of pneumonia can cause lasting damage to the airways.
- Whooping cough: Also known as pertussis, whooping cough can lead to bronchiectasis, especially in young children.
- Measles: Although less common due to vaccination, measles can cause lung damage that leads to bronchiectasis.
- Tuberculosis (TB): TB can cause significant damage to the lungs, resulting in bronchiectasis.
2.2. Are There Genetic Factors That Contribute to Bronchiectasis?
Genetic conditions can also increase the risk of developing bronchiectasis. Cystic fibrosis is the most well-known genetic cause, but other inherited conditions can also play a role.
- Cystic Fibrosis (CF): CF causes the body to produce thick, sticky mucus that can clog the airways, leading to infections and bronchiectasis. According to the Cystic Fibrosis Foundation, bronchiectasis affects 50%-75% of children with CF by 3-5 years of age.
- Primary Ciliary Dyskinesia (PCD): PCD is a genetic disorder that affects the function of cilia, the tiny hair-like structures that line the airways and help clear mucus. When cilia don’t work properly, mucus builds up, leading to infections and bronchiectasis. Studies indicate that up to 26% of children with PCD also develop bronchiectasis.
- Alpha-1 Antitrypsin Deficiency: This genetic condition results in a deficiency of alpha-1 antitrypsin, a protein that protects the lungs. The deficiency can lead to lung damage and bronchiectasis.
2.3. How Do Immune System Disorders Relate to Bronchiectasis?
Immune system disorders can weaken the body’s ability to fight off infections, increasing the risk of lung damage and bronchiectasis. Common immune disorders associated with bronchiectasis include:
- Common Variable Immunodeficiency (CVID): CVID is an immune disorder characterized by low levels of antibodies, making individuals more susceptible to infections. Research suggests that CVID is present 53% of the time in adults with bronchiectasis.
- Allergic Bronchopulmonary Aspergillosis (ABPA): ABPA is an allergic reaction to a fungus called Aspergillus, which can cause inflammation and damage in the lungs, leading to bronchiectasis.
- Rheumatoid Arthritis: This autoimmune disease can affect the lungs, causing inflammation and damage that may result in bronchiectasis.
2.4. What Other Lung Conditions Can Lead to Bronchiectasis?
Certain pre-existing lung conditions can also increase the risk of developing bronchiectasis. These conditions often involve chronic inflammation or obstruction of the airways.
- Chronic Obstructive Pulmonary Disease (COPD): COPD, which includes conditions like emphysema and chronic bronchitis, can damage the airways and increase the risk of bronchiectasis. Studies show that severe COPD is present 35%-50% of the time in adults with bronchiectasis.
- Severe Asthma: Chronic inflammation in the airways due to severe asthma can lead to structural changes and bronchiectasis. It is estimated that 25%-40% of adults with severe asthma also have bronchiectasis.
- Aspiration: Repeated aspiration of food or stomach contents into the lungs can cause inflammation and damage, leading to bronchiectasis.
- Bronchial Obstruction: Blockages in the airways, such as from tumors or foreign objects, can lead to bronchiectasis in the affected area of the lung.
3. What Are the Symptoms of Bronchiectasis?
The symptoms of bronchiectasis can vary in severity and may come and go. Common symptoms include a chronic cough, production of mucus, shortness of breath, and fatigue. Recognizing these symptoms early is crucial for timely diagnosis and management.
3.1. How Does Chronic Cough Manifest in Bronchiectasis?
Chronic cough is one of the hallmark symptoms of bronchiectasis. The cough is usually persistent and productive, meaning it produces mucus.
- Persistent Cough: The cough lasts for months or even years.
- Mucus Production: The cough is usually accompanied by the production of a significant amount of mucus, which can be clear, white, yellow, or green.
- Worse in the Morning: Coughing may be more severe in the morning as mucus accumulates overnight.
- Exacerbations: The cough may worsen during flare-ups or infections.
3.2. What Does the Mucus Produced in Bronchiectasis Look Like?
The mucus produced by individuals with bronchiectasis can vary in color and consistency, providing clues about potential infections or inflammation.
- Color: Mucus can be clear, white, yellow, green, or even blood-tinged.
- Consistency: It can range from thin and watery to thick and sticky.
- Amount: The amount of mucus produced can vary from small to large quantities.
- Odor: In some cases, the mucus may have a foul odor, especially during infections.
3.3. Why Does Shortness of Breath Occur in Bronchiectasis?
Shortness of breath, or dyspnea, is another common symptom of bronchiectasis. The damaged airways and mucus buildup can make it difficult to breathe, especially during physical activity or infections.
- Airflow Obstruction: Damaged airways can restrict airflow, making it harder to breathe.
- Mucus Plugging: Mucus can block the airways, further reducing airflow.
- Inflammation: Chronic inflammation in the lungs can contribute to shortness of breath.
- Reduced Lung Capacity: Over time, lung damage can reduce overall lung capacity.
3.4. How Does Bronchiectasis Cause Fatigue?
Fatigue is a common complaint among individuals with bronchiectasis. The chronic inflammation, persistent coughing, and difficulty breathing can all contribute to feelings of tiredness and exhaustion.
- Increased Work of Breathing: The body has to work harder to breathe, which can lead to fatigue.
- Chronic Inflammation: Ongoing inflammation can drain energy levels.
- Sleep Disruption: Frequent coughing and shortness of breath can disrupt sleep, leading to fatigue.
- Nutritional Deficiencies: Some individuals with bronchiectasis may have difficulty maintaining a healthy weight due to increased energy expenditure and decreased appetite, which can contribute to fatigue.
3.5. What Are Some Less Common Symptoms of Bronchiectasis?
In addition to the main symptoms, some individuals with bronchiectasis may experience other less common symptoms, such as:
- Wheezing: A whistling sound during breathing, caused by narrowed airways.
- Chest Pain: Discomfort or pain in the chest, especially during coughing or deep breathing.
- Weight Loss: Unintentional weight loss due to increased energy expenditure and decreased appetite.
- Clubbing of Fingers and Toes: A widening and rounding of the fingertips and toes, which can occur in chronic lung conditions.
- Frequent Respiratory Infections: Increased susceptibility to infections like pneumonia and bronchitis.
4. How Is Bronchiectasis Diagnosed?
Diagnosing bronchiectasis typically involves a combination of medical history, physical examination, and diagnostic tests. These tests help confirm the diagnosis, identify the extent of lung damage, and determine the underlying cause.
4.1. What Questions Will a Doctor Ask to Diagnose Bronchiectasis?
During a medical history assessment, a doctor will ask about your symptoms, medical history, and potential risk factors for bronchiectasis. Key questions may include:
- Symptom Onset: When did your symptoms start, and how have they changed over time?
- Cough Characteristics: How often do you cough, and what does the mucus look like?
- Medical History: Have you had any severe lung infections, such as pneumonia or tuberculosis?
- Family History: Is there a family history of cystic fibrosis, primary ciliary dyskinesia, or other lung conditions?
- Risk Factors: Do you have any conditions that might increase your risk, such as immune disorders or aspiration problems?
4.2. What Does a Physical Exam Involve When Bronchiectasis Is Suspected?
A physical examination can provide valuable clues about the presence of bronchiectasis. During the exam, the doctor will:
- Listen to Your Lungs: Using a stethoscope, the doctor will listen for abnormal lung sounds, such as wheezing, crackles, or decreased breath sounds.
- Check Your Vital Signs: The doctor will measure your heart rate, blood pressure, and oxygen saturation levels.
- Look for Clubbing: The doctor will examine your fingers and toes for signs of clubbing.
- Assess Your Overall Health: The doctor will evaluate your general health and look for any other signs of underlying conditions.
4.3. What Imaging Tests Are Used to Diagnose Bronchiectasis?
Imaging tests play a crucial role in diagnosing bronchiectasis and assessing the extent of lung damage.
- Chest X-Ray: A chest X-ray can help identify abnormalities in the lungs, such as widened airways or mucus plugging.
- High-Resolution Computed Tomography (HRCT) Scan: HRCT is the most sensitive imaging test for diagnosing bronchiectasis. It provides detailed images of the lungs, allowing doctors to visualize the damaged airways and assess the severity of the condition.
- Bronchoscopy: In some cases, a bronchoscopy may be performed to examine the airways directly. During this procedure, a thin, flexible tube with a camera is inserted into the airways to visualize any abnormalities and collect samples for testing.
4.4. What Lab Tests Are Conducted to Determine the Cause of Bronchiectasis?
Lab tests can help identify the underlying cause of bronchiectasis and guide treatment decisions. Common lab tests include:
- Sputum Culture: A sputum culture can identify bacteria or fungi in the mucus, helping to diagnose infections.
- Sweat Test: A sweat test is used to diagnose cystic fibrosis by measuring the amount of chloride in sweat.
- Blood Tests: Blood tests can help identify immune disorders, such as common variable immunodeficiency, and other conditions that may contribute to bronchiectasis.
- Genetic Testing: Genetic testing can be used to diagnose cystic fibrosis, primary ciliary dyskinesia, and other genetic conditions associated with bronchiectasis.
5. What Treatment Options Are Available for Bronchiectasis?
While there is no cure for bronchiectasis, various treatment options can help manage symptoms, prevent infections, and improve quality of life. Treatment typically involves a combination of airway clearance techniques, medications, and lifestyle modifications.
5.1. How Can Airway Clearance Techniques Help Manage Bronchiectasis?
Airway clearance techniques are essential for removing mucus from the lungs and preventing infections. These techniques include:
- Chest Physiotherapy: Chest physiotherapy involves techniques such as percussion (clapping on the chest), vibration, and postural drainage to loosen and remove mucus from the airways.
- High-Frequency Chest Wall Oscillation (HFCWO): HFCWO involves wearing an inflatable vest that vibrates the chest wall to loosen mucus.
- Positive Expiratory Pressure (PEP) Therapy: PEP therapy involves breathing through a device that creates resistance, helping to open the airways and mobilize mucus.
- Autogenic Drainage: Autogenic drainage is a breathing technique that uses different breathing depths and speeds to mobilize mucus from the small airways to the larger airways, where it can be coughed out.
- Active Cycle of Breathing Technique (ACBT): ACBT involves a combination of breathing control, thoracic expansion exercises, and forced expiratory techniques to clear mucus from the lungs.
5.2. What Medications Are Used to Treat Bronchiectasis?
Medications play a crucial role in managing symptoms, preventing infections, and reducing inflammation in individuals with bronchiectasis.
- Antibiotics: Antibiotics are used to treat bacterial infections in the lungs. They can be administered orally, intravenously, or through inhaled solutions.
- Bronchodilators: Bronchodilators help to open the airways and make it easier to breathe. They are often used to treat wheezing and shortness of breath.
- Mucolytics: Mucolytics help to thin the mucus, making it easier to cough up.
- Inhaled Corticosteroids: Inhaled corticosteroids can help reduce inflammation in the airways.
- Inhaled Hypertonic Saline: Inhaled hypertonic saline helps to hydrate the airways and loosen mucus.
5.3. Is Surgery an Option for Treating Bronchiectasis?
Surgery is rarely needed for bronchiectasis, but it may be considered in certain situations. Surgical options include:
- Lung Resection: In severe cases where bronchiectasis is localized to a specific area of the lung, surgical removal of the affected area may be considered.
- Lung Transplant: Lung transplantation may be an option for individuals with severe bronchiectasis who have not responded to other treatments.
5.4. What Lifestyle Changes Can Help Manage Bronchiectasis?
Lifestyle changes can play a significant role in managing bronchiectasis and improving overall health.
- Stay Hydrated: Drinking plenty of fluids helps to thin the mucus, making it easier to cough up.
- Avoid Irritants: Avoid exposure to smoke, pollutants, and other irritants that can worsen symptoms.
- Get Vaccinated: Get vaccinated against the flu and pneumonia to prevent infections.
- Exercise Regularly: Regular exercise can help improve lung function and overall fitness.
- Maintain a Healthy Diet: Eating a balanced diet can help support your immune system and maintain a healthy weight.
- Quit Smoking: If you smoke, quitting is essential for preventing further lung damage.
6. What Are the Potential Complications of Bronchiectasis?
Bronchiectasis can lead to various complications if not properly managed. These complications can affect lung function, overall health, and quality of life.
6.1. How Can Bronchiectasis Lead to Respiratory Failure?
Respiratory failure is a severe complication of bronchiectasis that occurs when the lungs are unable to adequately provide oxygen to the body or remove carbon dioxide.
- Progressive Lung Damage: Over time, bronchiectasis can cause progressive damage to the lungs, reducing their ability to function properly.
- Severe Infections: Frequent and severe lung infections can further impair lung function and lead to respiratory failure.
- Airway Obstruction: Mucus plugging and airway obstruction can prevent oxygen from reaching the lungs and carbon dioxide from being removed.
- Inflammation: Chronic inflammation in the lungs can contribute to respiratory failure.
6.2. What Is Pneumothorax, and How Is It Related to Bronchiectasis?
Pneumothorax, or a collapsed lung, is a condition in which air leaks into the space between the lung and the chest wall. It can occur as a complication of bronchiectasis due to the weakening of lung tissue.
- Weakened Lung Tissue: Bronchiectasis can weaken the lung tissue, making it more susceptible to rupture.
- Airway Damage: Damaged airways can lead to air leaks into the pleural space, causing a pneumothorax.
- Coughing: Vigorous coughing can also increase the risk of pneumothorax in individuals with bronchiectasis.
6.3. How Can Bronchiectasis Contribute to Heart Failure?
Heart failure can occur as a complication of bronchiectasis due to the increased strain on the heart.
- Pulmonary Hypertension: Chronic lung conditions like bronchiectasis can lead to pulmonary hypertension, a condition in which the pressure in the arteries that carry blood from the heart to the lungs becomes too high.
- Increased Cardiac Workload: Pulmonary hypertension can make it harder for the heart to pump blood to the lungs, increasing the workload on the heart.
- Right Ventricular Failure: Over time, the increased workload can cause the right ventricle of the heart to weaken and fail, leading to heart failure.
6.4. What Is Hemoptysis, and Why Does It Occur in Bronchiectasis?
Hemoptysis is the coughing up of blood or blood-tinged mucus. It can occur in bronchiectasis due to the inflammation and damage to the airways.
- Inflammation: Inflammation of the airways can cause small blood vessels to rupture, leading to bleeding.
- Infection: Infections can also cause inflammation and damage to the airways, increasing the risk of hemoptysis.
- Airway Damage: Damaged airways are more prone to bleeding.
7. How Can Bronchiectasis Be Prevented?
While it’s not always possible to prevent bronchiectasis, there are steps you can take to reduce your risk and protect your lungs.
7.1. What Vaccinations Can Help Prevent Bronchiectasis?
Vaccinations can help prevent infections that can lead to bronchiectasis. Recommended vaccinations include:
- Influenza Vaccine: The flu vaccine can help prevent influenza, a common cause of pneumonia.
- Pneumococcal Vaccine: The pneumococcal vaccine can help prevent pneumonia caused by Streptococcus pneumoniae bacteria.
- Pertussis Vaccine: The pertussis vaccine can help prevent whooping cough, which can lead to bronchiectasis, especially in young children.
- Measles, Mumps, and Rubella (MMR) Vaccine: The MMR vaccine can help prevent measles, which can cause lung damage that leads to bronchiectasis.
7.2. What Steps Can Be Taken to Prevent Lung Infections?
Preventing lung infections is crucial for reducing the risk of bronchiectasis. Key steps include:
- Practice Good Hygiene: Wash your hands frequently with soap and water to prevent the spread of germs.
- Avoid Contact with Sick Individuals: Stay away from people who are sick to reduce your risk of infection.
- Quit Smoking: Smoking damages the lungs and increases the risk of infections.
- Manage Underlying Conditions: Properly manage underlying conditions such as asthma, COPD, and immune disorders to reduce your risk of lung infections.
- Avoid Aspiration: Take steps to prevent aspiration, such as eating slowly and sitting upright after meals.
7.3. How Can Early Treatment of Lung Conditions Help Prevent Bronchiectasis?
Early treatment of lung conditions can help prevent the progression to bronchiectasis. Seek medical attention promptly if you experience symptoms of lung disease, such as chronic cough, shortness of breath, or frequent infections.
8. What Is the Prognosis for People With Bronchiectasis?
The prognosis for people with bronchiectasis can vary depending on the severity of the condition, the underlying cause, and the effectiveness of treatment. With proper management, many individuals with bronchiectasis can live full and active lives.
8.1. What Factors Influence the Long-Term Outlook for Bronchiectasis?
Several factors can influence the long-term outlook for bronchiectasis, including:
- Severity of the Condition: The extent of lung damage and the frequency of infections can affect the long-term prognosis.
- Underlying Cause: The underlying cause of bronchiectasis can influence the course of the disease. For example, individuals with cystic fibrosis may have a different prognosis than those with bronchiectasis caused by a previous infection.
- Treatment Adherence: Adhering to the prescribed treatment plan, including airway clearance techniques, medications, and lifestyle modifications, can improve the long-term outlook.
- Overall Health: Overall health and the presence of other medical conditions can also affect the prognosis.
8.2. What Is the Life Expectancy for Someone With Bronchiectasis?
Life expectancy for individuals with bronchiectasis can vary widely. With proper management and treatment, many people with bronchiectasis can live near-normal lifespans. However, severe cases with frequent infections and complications may have a shorter life expectancy.
8.3. How Can Quality of Life Be Improved for People With Bronchiectasis?
Quality of life can be significantly improved for people with bronchiectasis through effective management and lifestyle modifications.
- Symptom Management: Managing symptoms such as cough, shortness of breath, and fatigue can improve overall well-being.
- Preventing Infections: Preventing infections can reduce the risk of complications and improve quality of life.
- Pulmonary Rehabilitation: Pulmonary rehabilitation programs can help improve lung function, exercise tolerance, and overall quality of life.
- Support Groups: Joining a support group can provide emotional support and connect you with others who understand what you’re going through.
- Healthy Lifestyle: Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding irritants, can improve overall health and quality of life.
9. Bronchiectasis in Children: What Are the Key Considerations?
Bronchiectasis can occur in children, often due to infections or genetic conditions. Early diagnosis and management are crucial for preventing further lung damage and improving long-term outcomes.
9.1. What Are the Common Causes of Bronchiectasis in Children?
Common causes of bronchiectasis in children include:
- Cystic Fibrosis: CF is a major cause of bronchiectasis in children.
- Primary Ciliary Dyskinesia: PCD is another genetic condition that can lead to bronchiectasis in children.
- Severe Infections: Severe lung infections, such as pneumonia, whooping cough, and measles, can cause bronchiectasis in children.
- Aspiration: Repeated aspiration of food or stomach contents into the lungs can cause inflammation and damage, leading to bronchiectasis.
- Immune Disorders: Immune disorders can increase the risk of bronchiectasis in children.
9.2. How Does Bronchiectasis Affect Children Differently Than Adults?
Bronchiectasis can affect children differently than adults due to their developing lungs and immune systems.
- More Frequent Infections: Children with bronchiectasis may experience more frequent lung infections than adults.
- Growth and Development: Chronic lung disease can affect growth and development in children.
- Long-Term Lung Damage: Early lung damage can have long-term consequences for lung function.
9.3. What Are the Treatment Strategies for Children With Bronchiectasis?
Treatment strategies for children with bronchiectasis are similar to those for adults and include:
- Airway Clearance Techniques: Chest physiotherapy, HFCWO, and other airway clearance techniques are essential for removing mucus from the lungs.
- Medications: Antibiotics, bronchodilators, and other medications may be used to manage symptoms and prevent infections.
- Vaccinations: Vaccinations are crucial for preventing infections.
- Nutritional Support: Ensuring adequate nutrition is essential for growth and development.
- Parent Education: Educating parents about bronchiectasis and its management is crucial for successful treatment.
10. FAQs About Bronchiectasis
Here are some frequently asked questions about bronchiectasis, covering various aspects of the condition.
10.1. Is Bronchiectasis Contagious?
No, bronchiectasis itself is not contagious. However, the infections that can cause or worsen bronchiectasis can be contagious.
10.2. Can Bronchiectasis Be Cured?
Currently, there is no cure for bronchiectasis. However, with proper management and treatment, symptoms can be controlled, and quality of life can be improved.
10.3. What Are the Best Exercises for People With Bronchiectasis?
Regular exercise can help improve lung function and overall fitness. Recommended exercises include:
- Walking: Walking is a simple and effective way to improve cardiovascular health and lung function.
- Swimming: Swimming is a low-impact exercise that can improve lung capacity and endurance.
- Cycling: Cycling can help improve cardiovascular health and leg strength.
- Breathing Exercises: Breathing exercises, such as diaphragmatic breathing and pursed-lip breathing, can help improve lung function and reduce shortness of breath.
10.4. How Can I Manage My Cough With Bronchiectasis?
Managing your cough is an important part of bronchiectasis treatment. Tips for managing your cough include:
- Stay Hydrated: Drinking plenty of fluids helps to thin the mucus, making it easier to cough up.
- Use Airway Clearance Techniques: Chest physiotherapy, HFCWO, and other airway clearance techniques can help remove mucus from the lungs.
- Avoid Irritants: Avoid exposure to smoke, pollutants, and other irritants that can worsen your cough.
- Talk to Your Doctor: Your doctor may prescribe medications to help manage your cough.
10.5. What Should I Do If I Have a Flare-Up of Bronchiectasis Symptoms?
If you experience a flare-up of bronchiectasis symptoms, such as increased cough, mucus production, or shortness of breath, it’s important to seek medical attention promptly. Your doctor may prescribe antibiotics or other medications to treat the infection and manage your symptoms.
10.6. Are There Any Natural Remedies for Bronchiectasis?
While natural remedies may help to alleviate some symptoms of bronchiectasis, they should not be used as a substitute for medical treatment. Some natural remedies that may be helpful include:
- Honey: Honey has antibacterial and anti-inflammatory properties that may help to soothe a cough.
- Ginger: Ginger has anti-inflammatory properties that may help to reduce inflammation in the airways.
- Turmeric: Turmeric contains curcumin, which has anti-inflammatory and antioxidant properties.
- Eucalyptus Oil: Eucalyptus oil can help to open the airways and make it easier to breathe.
10.7. Can Bronchiectasis Cause Other Health Problems?
Yes, bronchiectasis can lead to other health problems, such as respiratory failure, pneumothorax, heart failure, and hemoptysis.
10.8. How Often Should I See My Doctor If I Have Bronchiectasis?
The frequency of doctor visits will depend on the severity of your condition and the effectiveness of your treatment. Your doctor will recommend a schedule that is appropriate for your individual needs.
10.9. What Questions Should I Ask My Doctor About Bronchiectasis?
When you see your doctor about bronchiectasis, it’s helpful to ask questions to better understand your condition and treatment options. Some questions you may want to ask include:
- What is the underlying cause of my bronchiectasis?
- What are my treatment options?
- How can I manage my symptoms?
- What are the potential complications of bronchiectasis?
- What lifestyle changes can I make to improve my health?
- How often should I see you for follow-up appointments?
10.10. Where Can I Find Support and Resources for People With Bronchiectasis?
There are many organizations that provide support and resources for people with bronchiectasis, including:
- The American Lung Association: The American Lung Association provides information, support, and advocacy for people with lung diseases.
- The Cystic Fibrosis Foundation: The Cystic Fibrosis Foundation provides information, support, and research funding for cystic fibrosis.
- The National Heart, Lung, and Blood Institute (NHLBI): The NHLBI provides information about lung diseases and other health topics.
Understanding bronchiectasis is key to managing the condition effectively, and WHAT.EDU.VN can help answer all of your questions!
Are you struggling to find reliable answers to your health questions? Do you need quick, trustworthy information without the hassle? At WHAT.EDU.VN, we provide a free platform where you can ask any question and receive expert answers. Don’t let uncertainty affect your health decisions. Visit WHAT.EDU.VN today and get the clarity you deserve. Contact us at 888 Question City Plaza, Seattle, WA 98101, United States. Whatsapp: +1 (206) 555-7890. Website: what.edu.vn.