It’s a common oversimplification to say depression is merely a result of a chemical imbalance in the brain. While neurochemistry plays a role, the reality of depression is far more intricate. Current research indicates that depression arises from a combination of factors, not just an excess or deficit of specific brain chemicals. These factors encompass impaired mood regulation within the brain, genetic predispositions, and the impact of stressful life experiences. It’s the interplay of these elements that is believed to trigger depression.
To be clear, chemical processes are indeed involved, but it’s not as simple as pinpointing one chemical being too low or another too high. Numerous chemicals, both inside and outside nerve cells, are at work. The system governing mood, perceptions, and life experiences is dynamic and comprised of millions, even billions, of chemical reactions.
This inherent complexity explains why individuals with seemingly similar depression symptoms may have fundamentally different underlying issues. Consequently, treatment effectiveness can vary significantly from person to person.
While scientific understanding of depression’s biology has advanced considerably, it’s still not complete. Significant progress includes identifying links between specific brain areas and depression’s effects, understanding neurotransmitters’ role in brain cell communication, and recognizing the influence of genetics and life events on depression risk and symptoms.
This article will delve into how different brain regions influence mood, a crucial aspect in understanding depression.
Brain Regions and Mood Regulation
Popular culture often places emotions in the heart, but science firmly locates them in the brain. Specific brain regions are instrumental in regulating mood. Researchers are increasingly focusing on nerve cell connections, nerve cell growth, and the function of nerve circuits as major contributors to depression, potentially more so than just the levels of individual brain chemicals.
Sophisticated brain imaging techniques like positron emission tomography (PET), single-photon emission computed tomography (SPECT), and functional magnetic resonance imaging (fMRI) provide unprecedented insights into the living brain. For instance, fMRI can track brain region responses during various activities, while PET and SPECT scans map neurotransmitter receptor distribution and density in specific brain areas.
Utilizing these technologies has deepened our understanding of which brain regions govern mood and how depression can affect other functions, such as memory. Key areas implicated in depression include the amygdala, thalamus, and hippocampus (refer to Figure 1).
Studies indicate that the hippocampus is smaller in some individuals with depression. For example, a study in The Journal of Neuroscience using fMRI examined 24 women with a history of depression. The hippocampus was, on average, 9% to 13% smaller in depressed women compared to their non-depressed counterparts. Furthermore, the more depressive episodes a woman experienced, the smaller her hippocampus appeared to be. Stress, a significant factor in depression, is believed to play a role in this hippocampal size reduction, as stress may inhibit the production of new neurons (nerve cells) in this region.
Researchers are actively investigating the potential connection between reduced neurogenesis (the creation of new neurons) in the hippocampus and depressed mood. Interestingly, the mechanism of antidepressants lends support to this theory. While these medications rapidly increase neurotransmitter concentrations in the brain, patients typically don’t experience symptom relief for several weeks. This delay has long puzzled experts if depression were solely due to low neurotransmitter levels, why isn’t improvement immediate upon neurotransmitter increase?
The answer may lie in the time it takes for nerves to grow and establish new connections, a process spanning weeks. Animal studies have indeed demonstrated that antidepressants stimulate nerve cell growth and branching in the hippocampus. This suggests that the true therapeutic value of these drugs may be in promoting neurogenesis, strengthening nerve cell connections, and enhancing communication within nerve circuits. If this is the case, future depression medications could be developed to specifically target neurogenesis, potentially offering patients faster relief than current treatments.
Figure 1: Brain Regions Implicated in Depression
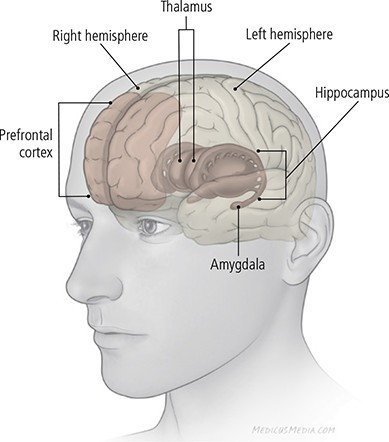 Illustration of key brain regions associated with depression: Amygdala, Hippocampus, and Basal Ganglia, highlighting their roles in mood regulation
Illustration of key brain regions associated with depression: Amygdala, Hippocampus, and Basal Ganglia, highlighting their roles in mood regulation
These regions are mirrored in both brain hemispheres and are interconnected. The illustration shows relative positions, not exact locations.
Amygdala: Located deep within the brain, the amygdala is central to processing emotions like anger, pleasure, sorrow, fear, and sexual arousal. Recalling emotionally charged memories, such as frightening events, activates the amygdala. In individuals experiencing sadness or clinical depression, amygdala activity is heightened, and this elevated activity can persist even after depression recovery. This increased activity may even contribute to amygdala enlargement.
Basal Ganglia (not pictured): The basal ganglia, another group of deep brain structures, interact with areas closer to the brain’s surface. They are thought to aid in movement facilitation and may be involved in memory, thought processes, and emotional processing. Some studies have observed shrinkage and other structural changes in the basal ganglia of people with depression.
Hippocampus: The hippocampus is crucial for long-term memory processing. The interplay between the hippocampus and amygdala might explain learned emotional responses. For instance, the hippocampus registers fear when encountering an aggressive dog, and the memory of this experience, stored within the hippocampus, can lead to future wariness of dogs. As mentioned, the hippocampus is often smaller in depressed individuals, and research suggests that prolonged exposure to stress hormones can hinder neuron growth in this brain region.
