When you hear the word testosterone, stereotypical images of hyper-masculine men, aggression, and impulsivity might spring to mind. However, the reality of testosterone’s role in the human body is far more nuanced and significantly more important than these outdated clichés suggest. In fact, many common perceptions surrounding testosterone are myths. This hormone is not just about “macho” behavior; it’s a critical player in a wide array of bodily functions and overall health for both men and women.
Did you know, for instance, that testosterone plays a surprising role in prostate cancer, a disease primarily affecting men? Or that women also require testosterone for various bodily processes? The truth is, testosterone is a complex hormone with diverse functions that extend far beyond common misconceptions.
This article delves into the essential question: What Does Testosterone Do? We will explore the multifaceted roles of this vital sex hormone, unraveling its primary benefits and dispelling myths to provide a comprehensive understanding of its importance in human health.
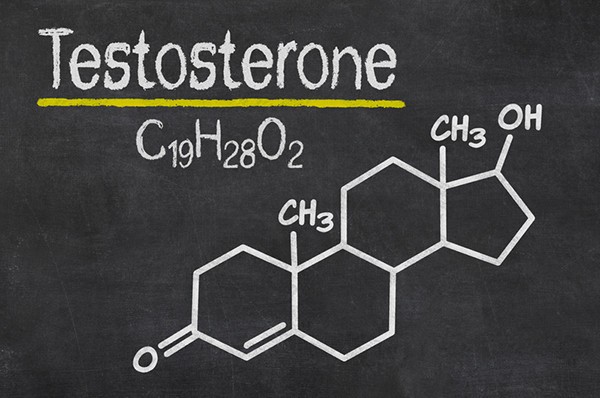
Understanding Testosterone: The Basics
Testosterone is classified as a sex hormone, belonging to a group of chemical messengers known as hormones. These messengers are produced by glands and organs and travel throughout the body, typically via the bloodstream, to regulate and influence a multitude of bodily processes.
In males, testosterone is the principal sex hormone, crucial for the development of male reproductive tissues like the testes and prostate, as well as the development of secondary sexual characteristics.
The production of testosterone is a carefully orchestrated process controlled by signals originating in the brain. The hypothalamus sends signals to the pituitary gland, located at the base of the brain. The pituitary gland, in turn, relays signals to the testes, instructing them to produce testosterone. This system operates on a “feedback loop” to maintain hormonal balance. When testosterone levels in the blood become too high, the brain signals the pituitary gland to reduce its signaling, thereby decreasing testosterone production.
 Close-up of a healthcare provider explaining hormone functions with a testosterone molecule model, emphasizing visual learning for patient education.
Close-up of a healthcare provider explaining hormone functions with a testosterone molecule model, emphasizing visual learning for patient education.
What Exactly Does Testosterone Do in the Body?
Testosterone exerts a wide range of effects throughout the body, playing numerous vital roles. These functions are essential for development, maintenance, and overall well-being. Key functions of testosterone include:
- Development of Male Reproductive Organs: Testosterone is critical for the formation of the penis and testes during fetal development.
- Pubertal Changes: During puberty, testosterone is responsible for the characteristic physical changes in boys, including the deepening of the voice.
- Hair Growth: Testosterone triggers the growth of facial and pubic hair during puberty. Interestingly, later in life, it can also contribute to male pattern baldness.
- Muscle Mass and Strength: Testosterone is a significant factor in promoting muscle growth and increasing strength. This is why it’s often associated with athletic performance and physical prowess.
- Bone Density and Strength: Testosterone plays a crucial role in bone growth and maintaining bone density, contributing to overall skeletal strength and reducing the risk of osteoporosis.
- Libido (Sex Drive): Testosterone is a primary driver of libido or sex drive in both men and women. It influences sexual desire and arousal.
- Sperm Production: Testosterone is essential for spermatogenesis, the process of sperm production in the testes, which is fundamental for male fertility.
- Mood Regulation: Testosterone may contribute to maintaining a stable mood and emotional well-being. Imbalances in testosterone levels can sometimes be linked to mood changes and irritability.
In adolescent boys, insufficient testosterone levels can impede normal masculinization. This can manifest as underdeveloped genitals, sparse facial and body hair, and a voice that doesn’t deepen as expected during puberty. Researchers continue to explore the full spectrum of testosterone’s functions, and it’s likely that more roles of this hormone are yet to be fully understood.
Testosterone’s Role in Women: Beyond Male Hormone Stereotypes
It’s a common misconception to think of testosterone as solely a male hormone. In reality, women also produce testosterone in their ovaries and adrenal glands. While present in lower amounts compared to men, testosterone is one of several androgens (male sex hormones) that play important roles in the female body. These roles are believed to include:
- Ovarian Function: Testosterone and other androgens are thought to be important for normal ovarian function and the complex processes involved in the female reproductive cycle.
- Bone Strength in Women: Similar to men, testosterone contributes to bone density and strength in women, playing a role in preventing osteoporosis.
- Sexual Behavior and Libido in Women: Testosterone is believed to influence sexual desire and behavior in women, contributing to a healthy libido. However, research in this area is ongoing, and the exact mechanisms are still being investigated.
- Potential Role in Brain Function: Emerging research suggests that androgens, including testosterone, may play a role in normal brain function in women, potentially affecting mood, sex drive, and cognitive functions. However, more research is needed to fully clarify these roles.
Maintaining a proper hormonal balance between testosterone (and other androgens) and estrogen is crucial for optimal ovarian function in women. While the precise details are still under investigation, it’s becoming increasingly clear that androgens, including testosterone, are not just “male” hormones but play vital and complex roles in women’s health as well.
Can Testosterone Levels Be Too High? Understanding Excess Testosterone
While low testosterone has gained significant attention, the issue of excessively high natural testosterone levels is less common in men. The perception of “testosterone excess” often gets misconstrued with behaviors like aggression or promiscuity. However, defining “normal” testosterone levels is complex as they can fluctuate significantly throughout the day and over time. Furthermore, behaviors attributed to high testosterone may often be unrelated to the hormone itself.
Much of our understanding of abnormally high testosterone comes from studying athletes who misuse anabolic steroids, testosterone, or related hormones to enhance muscle mass and athletic performance artificially.
Problems associated with artificially elevated testosterone levels in men can include:
- Paradoxical Reproductive Issues: Low sperm count, testicular shrinkage, and erectile dysfunction can occur – counterintuitive effects given testosterone’s role in sexual function.
- Cardiovascular Risks: Damage to the heart muscle and an increased risk of heart attack.
- Prostate Issues: Prostate enlargement, potentially leading to difficulty urinating.
- Liver Damage: Liver disease.
- Skin Problems: Acne.
- Fluid Retention: Edema, causing swelling in the legs and feet.
- Weight Gain: Potentially due to increased appetite.
- Cardiovascular Issues: High blood pressure and elevated cholesterol levels.
- Sleep Disturbances: Insomnia.
- Headaches.
- Muscle Mass Increase: While often desired, excessive muscle growth from artificial testosterone can be unhealthy.
- Blood Clot Risk: Increased risk of blood clots.
- Growth Stunting: In adolescents, high testosterone can prematurely stop bone growth, leading to stunted height.
- Behavioral Changes: Uncharacteristic aggression (though research is still evolving and not definitively proven), mood swings, euphoria, irritability, impaired judgment, and delusions.
In women, Polycystic Ovary Syndrome (PCOS) is a relatively common condition associated with high testosterone levels, affecting a significant percentage of premenopausal women. PCOS involves the development of multiple cysts on the ovaries and presents with symptoms such as irregular periods, reduced fertility, excessive hair growth (hirsutism) in male-like patterns, male-pattern baldness, skin darkening and thickening, weight gain, depression, and anxiety. Spironolactone, a diuretic medication, is sometimes used to manage PCOS symptoms by blocking the action of male sex hormones.
Women with high testosterone, whether due to conditions like PCOS or drug use, may experience a decrease in breast size and deepening of the voice, along with many of the health problems seen in men with excessive testosterone.
The Impact of Low Testosterone: Understanding Testosterone Deficiency
In recent years, there has been increasing focus on the effects of testosterone deficiency, particularly in men. As men age, testosterone levels naturally decline gradually, at a rate of about 1% to 2% per year. This decline is different from the rapid drop in estrogen levels experienced by women during menopause. Age-related testosterone reduction is due to several factors: the testes produce less testosterone, the pituitary gland sends fewer signals to stimulate testosterone production, and the liver produces more sex hormone-binding globulin (SHBG), which binds to testosterone, reducing the amount of active “free” testosterone available to the body.
It’s estimated that over a third of men over the age of 45 may have lower testosterone levels than considered typical. However, defining “optimal” testosterone levels remains complex and somewhat controversial.
Symptoms of testosterone deficiency in adult men can include:
- Reduced Hair: Decreased body and facial hair.
- Muscle Loss: Loss of muscle mass and strength.
- Sexual Dysfunction: Low libido, erectile dysfunction, smaller testicles, reduced sperm count, and infertility.
- Gynecomastia: Increased breast size.
- Vasomotor Symptoms: Hot flashes.
- Mood and Cognitive Changes: Irritability, poor concentration, and depression.
- Hair Loss: Loss of body hair.
- Bone Weakness: Brittle bones and an increased risk of fractures (osteoporosis).
For some men with testosterone deficiency, symptoms or conditions related to low testosterone may improve with testosterone replacement therapy. For instance, a man with osteoporosis and low testosterone might benefit from testosterone replacement to increase bone strength and reduce fracture risk.
Interestingly, women can also experience symptoms related to testosterone deficiency. Conditions affecting the pituitary or adrenal glands can lead to reduced testosterone production in women. Affected women may experience low libido, decreased bone strength, poor concentration, or depression.
Diseases and Conditions Affecting Testosterone Levels
Various diseases and conditions can disrupt testosterone production in both men and women.
In men, conditions affecting testosterone levels can involve:
- Testicular Issues: Direct injury to the testes, castration, infections, radiation treatment, chemotherapy, and tumors.
- Pituitary or Hypothalamic Issues: Tumors, medications (especially anabolic steroids), certain infections, and autoimmune conditions affecting the pituitary gland or hypothalamus.
- Genetic Conditions: Genetic diseases like Klinefelter syndrome (where a man has an extra X chromosome) and hemochromatosis (an inherited condition causing excessive iron accumulation, potentially affecting the pituitary gland).
In women, testosterone deficiency can result from:
- Diseases of the pituitary, hypothalamus, or adrenal glands.
- Removal of the ovaries.
- Estrogen therapy, which can increase SHBG levels, reducing free testosterone availability, similar to the age-related process in men.
Testosterone Therapy: When Is It Appropriate?
Testosterone therapy is an approved treatment for specific conditions, including delayed puberty in males and abnormally low testosterone production due to issues with the testes, pituitary gland, or hypothalamus.
Men may be considered candidates for testosterone therapy if they have significantly low levels of active (free) testosterone and experience symptoms like:
- Generalized weakness.
- Low energy levels.
- Debilitating frailty.
- Depression.
- Sexual dysfunction.
- Cognitive problems.
However, it’s important to note that many men with normal testosterone levels can experience similar symptoms, making a direct link between testosterone levels and symptoms not always clear-cut. This complexity leads to some debate about which men should receive testosterone supplementation.
Testosterone therapy may also be considered for women who have low testosterone levels and symptoms that might be linked to testosterone deficiency. However, the effectiveness and appropriateness of testosterone therapy to improve sexual function or cognitive function in postmenopausal women are still under investigation.
Risks and Considerations of Testosterone Therapy
Testosterone therapy, while beneficial for certain individuals, also carries potential risks and side effects.
Some possible side effects of testosterone treatment in both men and women include:
- Acne.
- Sleep apnea (disturbed breathing during sleep).
- Breast swelling or tenderness (gynecomastia).
- Edema (swelling in the ankles).
- Increased red blood cell count, which could increase the risk of blood clots.
While older concerns about testosterone therapy increasing the risk of prostate cancer have been largely disproven, testosterone can stimulate the growth of existing prostate cancer cells. Because prostate cancer is common, doctors often exercise caution when prescribing testosterone to men who may be at higher risk of undiagnosed prostate cancer. Men undergoing testosterone replacement therapy require careful monitoring for prostate health. It’s crucial to understand that while testosterone might fuel the growth of existing prostate cancer, it’s not definitively established that testosterone treatment causes prostate cancer.
For men with clearly documented low blood testosterone levels and symptoms strongly linked to this deficiency, the benefits of hormone replacement therapy often outweigh the potential risks. However, for most other individuals considering testosterone therapy, the decision should be made in consultation with a doctor, carefully weighing the potential benefits and risks in their specific situation.
The Bottom Line: Testosterone’s True Significance
Testosterone is far more than just a hormone associated with masculinity and aggression. It’s a vital hormone for both men and women, essential for a wide range of developmental and physiological functions. Maintaining the right testosterone balance is crucial for overall health and well-being.
Checking testosterone levels is a straightforward process involving a simple blood test. However, interpreting the results can be complex due to natural fluctuations in testosterone levels throughout the day. Measuring free testosterone levels in the morning is generally recommended for accuracy. Even when a consistently low testosterone level is confirmed through repeat testing, the decision to initiate testosterone replacement therapy, and the appropriate dosage, requires a detailed discussion with your physician. This conversation should consider individual symptoms, medical history, and potential risks and benefits to ensure the best course of action for your health.
Image: Zerbor/Dreamstime
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio
View all posts by Howard E. LeWine, MD