A coronary angiogram is a crucial diagnostic test that employs X-rays to visualize your heart’s blood vessels, known as the coronary arteries. This procedure is typically performed to determine if there are any blockages or narrowings in these vital arteries, often as a key step in diagnosing coronary artery disease.
The coronary angiogram is a component of a broader set of cardiac assessments and treatments referred to as cardiac catheterization. This technique involves the insertion of one or more thin, flexible tubes, called catheters, into the major blood vessels and heart. It requires a small incision in the skin. Importantly, during a coronary angiogram, if blockages are discovered, treatments like angioplasty and stenting can often be performed immediately to open the obstructed arteries.
In some instances, a coronary CT angiogram (CCTA), utilizing a computerized tomography (CT) scanner, can be used to examine the heart’s blood vessels. This non-invasive method doesn’t require catheter insertion. A CCTA can help determine if a cardiac catheterization-based angiogram is necessary. However, it’s important to note that blockages or narrowings cannot be treated during a CT angiogram. If a CCTA reveals an issue, a traditional coronary angiogram with catheterization is typically required for intervention.
This article will primarily focus on the coronary angiogram performed using cardiac catheterization, providing a comprehensive overview of this important medical procedure.
Why Might You Need an Angiogram?
A coronary angiogram is primarily performed to detect narrowed or blocked blood vessels in the heart. Your healthcare provider might recommend a coronary angiogram if you are experiencing certain symptoms or have specific risk factors, including:
- Chest pain (angina): Unexplained chest pain, particularly if suspected to be heart-related.
- Unexplained pain: Pain in the chest, jaw, neck, or arm that cannot be attributed to other causes.
- Known blood vessel issues: If you have a known history of blood vessel problems.
- Congenital heart defects: To assess heart problems present from birth.
- Abnormal stress test results: Irregular findings during an exercise stress test.
- Chest injury: Following a chest injury to evaluate potential heart or blood vessel damage.
- Heart valve disease requiring surgery: To assess coronary arteries before heart valve surgery.
Generally, an angiogram is considered after non-invasive heart tests, such as electrocardiograms (ECG), echocardiograms, or stress tests, have been conducted to initially evaluate heart health.
Understanding the Risks Associated with Angiograms
Like any medical procedure involving the heart and blood vessels, a coronary angiogram carries some risks. However, it’s crucial to understand that major complications are infrequent. Potential risks and complications can include:
- Blood vessel injury: Damage to the blood vessel at the insertion site.
- Excessive bleeding: Bleeding from the incision site or internally.
- Heart attack: Though rare, a heart attack can occur during or after the procedure.
- Infection: Infection at the catheter insertion site.
- Arrhythmias: Irregular heart rhythms.
- Kidney damage: The contrast dye used can potentially affect kidney function, especially in individuals with pre-existing kidney issues.
- Allergic reactions: Reactions to the contrast dye or medications used during the procedure.
- Stroke: A rare but serious complication.
Preparing for Your Angiogram Procedure
In emergency situations, a coronary angiogram may be performed without extensive preparation time. However, when the procedure is scheduled in advance, your healthcare team will provide detailed instructions on how to prepare. Typical preparation guidelines include:
- Fasting: You will be instructed to abstain from eating or drinking for several hours before the test. Your medical team will specify the exact time to stop.
- Medications: Discuss your regular medications with your doctor. Bring a comprehensive list of your medications, including dosages, to the hospital.
- Diabetes management: Inform your team if you have diabetes as your insulin or other diabetes medications may need adjustment before the angiogram.
What to Expect During the Angiogram Procedure
Before the Procedure
A coronary angiogram is performed in a hospital or specialized medical center, typically in a catheterization laboratory, often referred to as a “cath lab”. Before the procedure commences, your healthcare team will review your medical history, current medications, and any allergies you may have.
You will be asked to change into a hospital gown and empty your bladder. Remove any contact lenses, eyeglasses, jewelry, and hairpins.
Your blood pressure and pulse will be checked. Electrodes, small sticky patches, will be attached to your chest, and sometimes arms or legs, to monitor your heartbeat throughout the procedure and afterward.
A healthcare professional may need to shave a small area of hair at the catheter insertion site, which is then cleaned and numbed with a local anesthetic.
During the Procedure
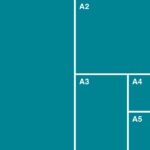
Cardiac catheterization procedure approaches
During a cardiac catheter procedure, a doctor inserts a flexible tube called a catheter into a blood vessel, commonly in the wrist artery (radial artery) or the groin artery (femoral artery), guiding it to the heart.
During the coronary angiogram itself, you will lie on your back on an X-ray table. Straps will be placed across your chest and legs to ensure your safety and stability on the table.
An intravenous (IV) line will be inserted into a vein in your forearm or hand. Sedative medication is administered through the IV to help you relax and remain calm during the test. This medication may induce drowsiness.
The level of sedation will depend on the reason for the angiogram and your overall health status. You may be fully conscious, lightly sedated, or, in some cases, placed under general anesthesia (a sleep-like state) using a combination of medications.
The doctor will make a small incision to access an artery, typically in the leg or wrist. A thin, flexible catheter is then inserted into the artery and carefully guided towards your heart. You should not feel the catheter moving within your body.
Once the catheter reaches the correct position, a contrast dye is injected through the catheter into the heart’s blood vessels. X-ray images are captured as the dye flows, creating angiograms. These images allow the medical team to visualize blood flow and identify any blockages or narrowings in the arteries, indicated by the dye not flowing properly through a vessel.
An uncomplicated coronary angiogram typically takes about an hour or longer to complete. The duration can vary depending on whether additional heart tests or treatments, such as angioplasty and stenting, are performed during the same procedure. If a blockage is detected, a balloon catheter may be advanced to widen the artery, and a stent (a small mesh tube) may be implanted to maintain artery openness.
Upon completion of the test or treatment, the catheter is removed. The small incision may be closed with a clamp or a small plug to prevent bleeding.
After the Procedure
Following the coronary angiogram, you will be moved to a recovery area where your healthcare team will closely monitor your heart rate, blood pressure, and oxygen levels.
If the catheter was inserted in your leg, you will need to lie flat for several hours to minimize the risk of bleeding. The insertion site may be tender, and you might experience bruising or a small bump.
Some patients are discharged on the same day after an angiogram, while others may require a hospital stay for a day or more, depending on the procedure’s findings and any treatments performed.
During your recovery period, it’s important to follow these general recommendations:
- Hydration: Drink plenty of fluids to help flush the contrast dye out of your system.
- Rest: Avoid strenuous activities and heavy lifting for several days.
- Hygiene: Ask your healthcare team about when you can bathe or shower.
- Medications: Take all prescribed medications as instructed.
Your healthcare team will provide specific guidance on when you can return to work and resume your normal daily activities.
Contact your healthcare provider if you experience any of the following:
- Chest pain or shortness of breath
- Bleeding, new bruising, swelling, or increasing pain at the catheter site
- Signs of infection, such as fever
- Drainage or color changes (red, purple, or brown depending on skin tone) around the incision site
- Changes in temperature or color in the leg or arm used for the procedure
- Weakness or numbness in a leg or arm
Seek immediate medical attention (call 911 or your local emergency number) if:
- The catheter insertion site continues to bleed and doesn’t stop with direct pressure.
Understanding Your Angiogram Results
A coronary angiogram provides detailed information about blood flow through your heart arteries. The results help your healthcare team:
- Identify blockages or narrowings: Pinpoint any obstructions in the coronary arteries.
- Assess blood flow reduction: Determine the extent to which blood flow to and from the heart is restricted.
- Detect atherosclerosis: Identify the buildup of plaque (fats, cholesterol, and other substances) on artery walls.
- Evaluate previous heart surgery outcomes: Check the effectiveness of prior heart surgeries.
This crucial information enables your healthcare team to develop the most effective treatment plan for your specific heart condition.
Clinical Trials and Angiograms
Explore Mayo Clinic studies for further research and advancements in tests and procedures like angiograms, aimed at improving prevention, detection, treatment, and management of heart conditions.