Atrial fibrillation (AFib) is a common heart condition characterized by an irregular and often rapid heart rhythm. Also known as AF or AFib, this arrhythmia occurs when the upper chambers of the heart, called the atria, beat chaotically and asynchronously with the lower chambers, the ventricles. This uncoordinated beating can lead to a variety of symptoms and health complications, making it crucial to understand what AFib is and how it impacts your health.
Living with AFib can be unsettling, as described by patients:
“My heart feels like it’s fluttering, skipping beats, and sometimes pounding. It’s especially noticeable when I’m active, like climbing stairs or bending over.”
“Suddenly, I felt dizzy, weak, and extremely tired. My heart was racing, and I felt short of breath, like I couldn’t get enough air.”
“I was surprised to learn I had AFib because I didn’t feel anything unusual. It was detected during a routine check-up, which I’m grateful for.”
These experiences highlight the variability of AFib symptoms, ranging from noticeable palpitations to being completely asymptomatic. Regardless of the presence of symptoms, understanding the underlying mechanisms and potential risks of AFib is vital for proactive health management.
How Atrial Fibrillation Affects Your Heart
In a healthy heart, electrical signals coordinate regular contractions of the atria and ventricles, ensuring efficient blood flow. During AFib, these electrical signals become erratic and rapid, causing the atria to quiver or fibrillate instead of contracting effectively. This leads to several issues:
- Inefficient Pumping: The atria do not pump blood effectively into the ventricles.
- Blood Pooling: Blood can pool in the atria, increasing the risk of clot formation.
- Irregular Heartbeat: The ventricles also beat irregularly in response to the chaotic atrial signals, though often at a slower rate than the atria.
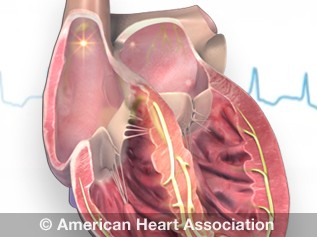 Atrial fibrillation (AFib) illustration showing irregular electrical signals in the atria leading to a quivering heart rhythm.
Atrial fibrillation (AFib) illustration showing irregular electrical signals in the atria leading to a quivering heart rhythm.
This irregular rhythm and potential for blood clots are the primary concerns associated with AFib. If a blood clot forms in the atria and travels to the brain, it can block blood flow and cause a stroke. In fact, AFib is estimated to be responsible for 15% to 20% of all strokes. This risk of stroke is why blood thinners are often prescribed for individuals with AFib.
Beyond stroke, untreated AFib can double the risk of heart-related deaths and significantly increase the risk of heart failure and other cardiovascular complications. Despite these serious risks, many people are unaware of the significance of AFib and the importance of seeking diagnosis and treatment.
Stages of Atrial Fibrillation: A Progressive Condition
AFib is often considered a progressive condition, meaning it can worsen over time. Understanding the stages of AFib can help in early detection, prevention, and effective management:
Stage 1: At Risk for AFib
In this stage, individuals have not been diagnosed with AFib, but they may have risk factors that increase their likelihood of developing it. These risk factors can include high blood pressure, heart disease, obesity, sleep apnea, and excessive alcohol consumption. This stage is crucial for preventative measures. Consulting with a healthcare professional to assess risk factors and adopt a heart-healthy lifestyle can be beneficial.
Stage 2: Pre-Atrial Fibrillation (Pre-AFib)
Pre-AFib is characterized by the presence of structural or electrical abnormalities in the heart that may predispose an individual to AFib, even without a formal diagnosis. At this stage, irregular heartbeats may not be consistently present or easily detectable, but underlying heart changes are occurring. Doctors may recommend closer monitoring and early interventions to slow or halt potential progression to AFib.
Stage 3: Atrial Fibrillation (AFib)
This is the stage of diagnosed AFib. Individuals in this stage experience episodes of irregular heart rhythm that are confirmed through medical testing, such as an electrocardiogram (ECG or EKG). The severity of AFib and the frequency and duration of episodes can vary significantly among individuals. Treatment at this stage focuses on managing heart rhythm and rate, preventing blood clots and stroke, and addressing underlying health conditions. Treatment options can include medications, lifestyle modifications, and in some cases, procedures or surgery.
Stage 4: Permanent Atrial Fibrillation
Permanent AFib is diagnosed when AFib is continuously present and cannot be effectively controlled with medications or procedures aimed at restoring normal heart rhythm. While normal rhythm cannot be restored, management at this stage focuses on controlling heart rate, preventing blood clots and stroke, and managing symptoms and other co-existing health conditions to improve quality of life and reduce risks.
Recognizing these stages underscores the importance of early detection and continuous management of AFib. Understanding your stage of AFib allows for informed discussions with your healthcare provider to develop the most appropriate treatment and management plan.
Diagnosis and Treatment for Atrial Fibrillation
Early diagnosis and effective treatment of AFib are critical for reducing the risk of serious complications and improving outcomes.
How is AFib Diagnosed?
Diagnosing AFib typically involves:
- Electrocardiogram (ECG/EKG): This is the primary diagnostic tool, recording the heart’s electrical activity and detecting irregular rhythms.
- Holter Monitor: A portable ECG that records heart rhythm over 24-48 hours or longer to capture intermittent AFib episodes.
- Event Recorder: A device worn for up to a month to record heart rhythm when symptoms occur.
- Echocardiogram: An ultrasound of the heart to assess its structure and function and rule out other heart conditions.
Treatment Options for AFib
Treatment strategies for AFib are tailored to the individual and may include:
- Medications:
- Rate Control Medications: To slow down the heart rate to a normal range.
- Rhythm Control Medications: To restore and maintain a normal heart rhythm.
- Blood Thinners (Anticoagulants): To prevent blood clot formation and reduce stroke risk.
- Catheter Ablation: A procedure to destroy the heart tissue causing the abnormal electrical signals.
- Cardioversion: A procedure to reset the heart rhythm, either with medication or electrical shock.
- Lifestyle Modifications: Managing risk factors such as high blood pressure, obesity, sleep apnea, and adopting a heart-healthy diet and exercise routine.
Seeking timely medical attention if you suspect you might have AFib is crucial. Effective treatments are available to manage AFib, reduce risks, and improve your overall health and well-being. If you are concerned about atrial fibrillation, consult with your healthcare provider to discuss your symptoms, risk factors, and appropriate diagnostic and treatment options.