Breast cancer is a disease where cells in the breast grow uncontrollably, and understanding it is crucial for early detection and effective treatment. At WHAT.EDU.VN, we aim to provide clear and accessible information about this complex topic, empowering you with knowledge regarding breast cancer awareness and screening. Learn about breast cancer symptoms, diagnosis, and treatment options.
1. Understanding How Breast Cancer Starts
Breast cancer predominantly affects women, although it’s essential to recognize that breast cancer in men is also possible. The genesis of cancer lies in the uncontrolled proliferation of cells. It’s crucial to remember that the majority of breast lumps are benign, meaning they are non-cancerous and do not spread. However, some benign breast conditions can increase the risk of developing breast cancer in the future.
Any noticeable changes or lumps in the breast should be evaluated by a healthcare professional to determine whether they are benign or malignant and to assess any potential impact on future cancer risk. Understanding non-cancerous breast conditions is vital for informed decision-making.
2. Pinpointing Where Breast Cancer Originates
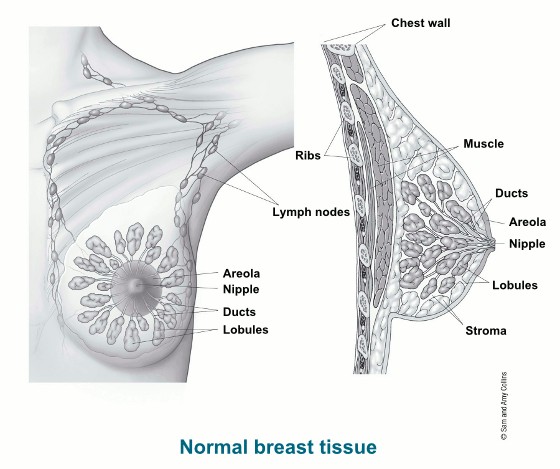
Breast cancer can arise from various parts of the breast. Each breast consists mainly of glands (lobules), ducts, and fatty tissue, overlying the upper ribs and chest muscles. The primary function of the breast in women is to produce and deliver milk for newborns.
Let’s explore the specific areas where breast cancer can begin:
- Lobules: These are the glands responsible for milk production, and cancers originating here are termed lobular cancers.
- Ducts: These are small canals that transport milk from the lobules to the nipple, representing the most common site for breast cancer to develop. Cancers starting here are known as ductal cancers.
- Nipple: This is the opening on the breast’s surface where milk exits. Paget’s disease of the nipple, a less common form of breast cancer, can originate here.
- Fat and Connective Tissue (Stroma): These tissues surround and support the ducts and lobules. Phyllodes tumors, a less frequent type of breast cancer, can arise in the stroma.
- Blood and Lymph Vessels: These vessels are also present in the breast. Angiosarcoma, a rare type of breast cancer, can develop in the lining of these vessels.
While uncommon, some cancers originate in other breast tissues, such as sarcomas and lymphomas, but these are not typically classified as breast cancers. Understanding the different types of breast cancer is essential for accurate diagnosis and treatment.
3. Understanding The Mechanisms of Breast Cancer Spread
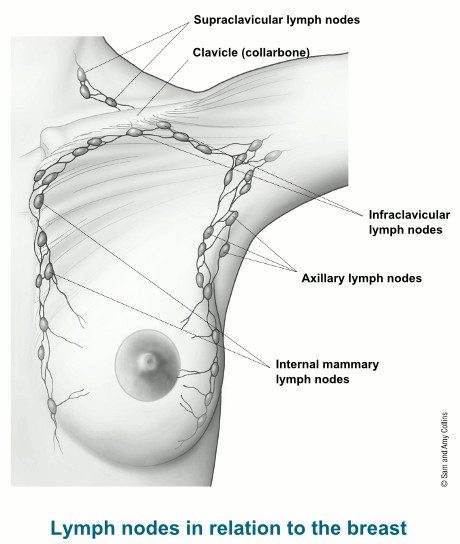
Breast cancer can spread through the bloodstream or lymphatic system, allowing cancer cells to reach other areas of the body.
The lymphatic system, integral to the body’s immune response, comprises lymph nodes, ducts, vessels, and organs that transport lymph fluid throughout the body. This fluid contains tissue by-products, waste, and immune cells.
Lymph vessels drain fluid away from the breast, and cancer cells can enter these vessels and proliferate in lymph nodes. The primary drainage pathways include:
- Axillary Lymph Nodes: Located under the arm.
- Internal Mammary Lymph Nodes: Situated inside the chest near the breastbone.
- Supraclavicular and Infraclavicular Lymph Nodes: Found around the collarbone.
The presence of cancer cells in lymph nodes increases the likelihood of metastasis to other parts of the body. However, not all individuals with affected lymph nodes develop metastases, and some without cancer cells in their lymph nodes may develop metastases later. Being aware of the stages of breast cancer can help in understanding the progression and treatment options.
4. Exploring Different Types of Breast Cancer
Breast cancer encompasses various types, classified based on the specific cells affected. Most breast cancers are carcinomas, with adenocarcinomas being the most prevalent. These originate in the gland cells of milk ducts or lobules. Rarer forms include angiosarcoma and sarcoma, which arise from different breast cells and are not considered breast cancers.
Breast cancers are also categorized by specific proteins or genes they express. Following a biopsy, breast cancer cells undergo testing for estrogen and progesterone receptors, as well as the HER2 gene or protein. Additionally, tumor cells are examined to determine their grade. These factors aid in determining the cancer stage and appropriate treatment strategies.
5. Identifying Risk Factors for Breast Cancer
Understanding the factors that can increase the risk of breast cancer is essential for prevention and early detection. While some risk factors are beyond our control, such as genetics and age, others can be modified through lifestyle choices.
5.1. Non-Modifiable Risk Factors
These are factors that cannot be changed.
- Age: The risk of breast cancer increases with age. Most cases are diagnosed after age 50.
- Genetics: Inherited genetic mutations, such as BRCA1 and BRCA2, significantly increase the risk.
- Family History: Having a close relative with breast cancer increases your risk.
- Personal History: A previous diagnosis of breast cancer or certain non-cancerous breast conditions can increase risk.
- Race and Ethnicity: White women are slightly more likely to develop breast cancer than African American women, but African American women are more likely to die from it.
- Early Menarche: Starting menstruation at a young age (before 12) slightly increases risk.
- Late Menopause: Starting menopause at a later age (after 55) slightly increases risk.
- Dense Breast Tissue: Women with dense breast tissue have a higher risk.
- Exposure to DES: Women whose mothers took diethylstilbestrol (DES) during pregnancy have a slightly increased risk.
5.2. Modifiable Risk Factors
These are factors that can be changed through lifestyle choices.
- Obesity: Being overweight or obese, especially after menopause, increases risk.
- Physical Inactivity: Lack of regular exercise increases risk.
- Alcohol Consumption: Drinking alcohol increases risk, with the risk increasing with the amount of alcohol consumed.
- Hormone Therapy: Long-term use of hormone therapy after menopause increases risk.
- Smoking: Smoking is linked to a higher risk of breast cancer, especially in premenopausal women.
- Childbearing: Women who have not had children or who had their first child after age 30 have a slightly higher risk.
- Breastfeeding: Breastfeeding can lower the risk of breast cancer.
- Exposure to Radiation: Exposure to radiation, such as from radiation therapy, increases risk.
Understanding these risk factors can help individuals make informed decisions about their health and lifestyle. Regular check-ups and screenings are crucial for early detection.
6. Recognizing Breast Cancer Symptoms
Early detection of breast cancer significantly improves treatment outcomes. Recognizing potential symptoms is crucial for prompt medical evaluation.
Common signs and symptoms of breast cancer include:
- New Lump or Mass: A lump or mass in the breast or underarm area is a common symptom. It’s often painless but can sometimes be tender.
- Change in Breast Size or Shape: Noticeable changes in the size, shape, or contour of the breast.
- Skin Changes: Redness, swelling, dimpling, or thickening of the breast skin. This may resemble the texture of an orange peel (peau d’orange).
- Nipple Changes: Nipple retraction (turning inward), scaling, crusting, or discharge (other than breast milk).
- Pain in the Breast or Nipple: Persistent pain in the breast or nipple that doesn’t go away.
- Swelling in the Underarm Area: Swelling or lumps in the lymph nodes under the arm or around the collarbone.
It’s important to note that these symptoms can also be caused by non-cancerous conditions. However, any new or persistent changes should be evaluated by a healthcare professional.
7. Breast Cancer Screening Methods
Regular screening plays a critical role in detecting breast cancer early, when treatment is most effective. Different screening methods are available, each with its benefits and limitations.
7.1. Mammograms
A mammogram is an X-ray of the breast used to detect tumors or other abnormalities. It’s the most common and effective screening tool for breast cancer.
- Benefits: Can detect tumors before they are large enough to be felt, reducing the risk of advanced-stage cancer.
- Limitations: May not be as effective in women with dense breast tissue. Can sometimes lead to false-positive results.
- Recommendations: The American Cancer Society recommends that women aged 45 to 54 get mammograms every year. Women 55 and older can switch to every other year or continue yearly screening.
7.2. Clinical Breast Exams
A clinical breast exam is a physical examination of the breasts performed by a healthcare professional.
- Benefits: Can detect lumps or abnormalities that may not be visible on a mammogram.
- Limitations: Less effective than mammograms in detecting early-stage cancer.
- Recommendations: Should be part of a routine medical check-up.
7.3. Breast Self-Exams
A breast self-exam involves checking your breasts for any changes or abnormalities.
- Benefits: Helps women become familiar with their breasts and detect changes early.
- Limitations: Less effective than mammograms and clinical breast exams.
- Recommendations: Women should be familiar with how their breasts normally look and feel and report any changes to their healthcare provider.
7.4. Breast MRI
A breast MRI (magnetic resonance imaging) uses magnetic fields and radio waves to create detailed images of the breast.
- Benefits: More sensitive than mammograms, especially in women with dense breast tissue or a high risk of breast cancer.
- Limitations: More expensive than mammograms and may lead to more false-positive results.
- Recommendations: Recommended for women with a high risk of breast cancer, such as those with BRCA1 or BRCA2 mutations.
7.5. Ultrasound
An ultrasound uses sound waves to create images of the breast.
- Benefits: Can help distinguish between solid masses and fluid-filled cysts.
- Limitations: Less effective than mammograms in detecting early-stage cancer.
- Recommendations: Often used as a follow-up test after an abnormal mammogram.
Choosing the right screening method depends on individual risk factors and healthcare provider recommendations.
8. Understanding Breast Cancer Diagnosis
If a screening test or symptom raises suspicion of breast cancer, further diagnostic tests are needed to confirm the diagnosis and determine the characteristics of the cancer.
8.1. Biopsy
A biopsy is the removal of a small sample of breast tissue for examination under a microscope. It’s the only way to definitively diagnose breast cancer.
- Types of Biopsies:
- Fine Needle Aspiration (FNA): Uses a thin needle to draw fluid or cells from a suspicious area.
- Core Needle Biopsy: Uses a larger needle to remove a small core of tissue.
- Incisional Biopsy: Removes a small piece of a suspicious area.
- Excisional Biopsy: Removes the entire suspicious area.
8.2. Imaging Tests
Imaging tests, such as mammograms, ultrasounds, and MRIs, can help determine the size and location of the tumor and whether it has spread to other areas.
8.3. Blood Tests
Blood tests can help assess overall health and detect any signs of cancer spread.
8.4. Genetic Testing
Genetic testing may be recommended for individuals with a high risk of breast cancer, such as those with a family history of the disease or known genetic mutations.
9. Staging Breast Cancer
Staging is the process of determining the extent of the cancer, including the size of the tumor and whether it has spread to lymph nodes or other parts of the body. The stage of breast cancer helps determine the best treatment options and predict prognosis.
The staging system used for breast cancer is the TNM system:
- T (Tumor): Describes the size and extent of the primary tumor.
- N (Nodes): Indicates whether the cancer has spread to nearby lymph nodes.
- M (Metastasis): Indicates whether the cancer has spread to distant parts of the body.
Based on the TNM classification, breast cancer is assigned a stage from 0 to IV:
- Stage 0: Cancer is confined to the ducts or lobules (in situ).
- Stage I: Cancer is small and has not spread to lymph nodes.
- Stage II: Cancer is larger or has spread to a few nearby lymph nodes.
- Stage III: Cancer has spread to multiple lymph nodes or surrounding tissues.
- Stage IV: Cancer has spread to distant parts of the body (metastatic).
10. Breast Cancer Treatment Options
Treatment for breast cancer depends on several factors, including the type and stage of the cancer, hormone receptor status, HER2 status, and overall health of the patient. Common treatment options include:
10.1. Surgery
Surgery is often the first step in treating breast cancer. The goal of surgery is to remove the tumor and any nearby lymph nodes that may contain cancer cells.
- Types of Surgery:
- Lumpectomy: Removal of the tumor and a small amount of surrounding tissue.
- Mastectomy: Removal of the entire breast.
- Simple Mastectomy: Removal of the entire breast.
- Modified Radical Mastectomy: Removal of the entire breast and nearby lymph nodes.
- Skin-Sparing Mastectomy: Removal of breast tissue but preserves the skin envelope.
- Nipple-Sparing Mastectomy: Removal of breast tissue but preserves the skin and nipple.
10.2. Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It may be used after surgery to kill any remaining cancer cells or to treat cancer that has spread to other areas.
- Types of Radiation Therapy:
- External Beam Radiation: Radiation is delivered from a machine outside the body.
- Brachytherapy: Radioactive seeds or pellets are placed inside the breast near the tumor.
10.3. Chemotherapy
Chemotherapy uses drugs to kill cancer cells throughout the body. It may be used before surgery to shrink the tumor or after surgery to kill any remaining cancer cells.
- Types of Chemotherapy:
- Adjuvant Chemotherapy: Given after surgery to reduce the risk of recurrence.
- Neoadjuvant Chemotherapy: Given before surgery to shrink the tumor.
10.4. Hormone Therapy
Hormone therapy is used to treat breast cancers that are hormone receptor-positive (ER-positive or PR-positive). It works by blocking the effects of estrogen or progesterone on cancer cells.
- Types of Hormone Therapy:
- Tamoxifen: Blocks estrogen receptors.
- Aromatase Inhibitors: Reduce the amount of estrogen produced in the body.
10.5. Targeted Therapy
Targeted therapy uses drugs that target specific proteins or genes that are involved in cancer growth. It may be used to treat breast cancers that are HER2-positive.
- Types of Targeted Therapy:
- Trastuzumab (Herceptin): Targets the HER2 protein.
- Pertuzumab (Perjeta): Targets the HER2 protein.
10.6. Immunotherapy
Immunotherapy uses drugs to help the body’s immune system fight cancer. It may be used to treat certain types of breast cancer, such as triple-negative breast cancer.
- Types of Immunotherapy:
- PD-1 Inhibitors: Block the PD-1 protein, which helps cancer cells evade the immune system.
11. Understanding Breast Reconstruction
Breast reconstruction is a surgical procedure to rebuild the breast after a mastectomy. It can improve body image and quality of life.
11.1. Types of Breast Reconstruction
- Implant Reconstruction: Uses silicone or saline implants to create a breast shape.
- Tissue Flap Reconstruction: Uses tissue from another part of the body (such as the abdomen, back, or thighs) to create a breast shape.
- DIEP Flap: Uses skin and fat from the lower abdomen.
- Latissimus Dorsi Flap: Uses skin and muscle from the back.
- TRAM Flap: Uses skin, fat, and muscle from the abdomen.
12. Addressing Common Concerns
Many questions and concerns can arise when dealing with breast cancer.
| Question | Answer |
|---|---|
| Can men get breast cancer? | Yes, although it’s rare. Men have breast tissue that can develop cancer. |
| Is breast cancer hereditary? | About 5-10% of breast cancers are linked to inherited genetic mutations, such as BRCA1 and BRCA2. |
| Does breast cancer always cause a lump? | No, breast cancer can sometimes present with other symptoms, such as skin changes, nipple discharge, or swelling in the underarm area. |
| Is breast cancer always fatal? | No, early detection and treatment have significantly improved survival rates. |
| Can lifestyle changes reduce the risk of recurrence? | Yes, maintaining a healthy weight, exercising regularly, limiting alcohol consumption, and not smoking can help reduce the risk of recurrence. |
| What is triple-negative breast cancer? | Triple-negative breast cancer is a type of breast cancer that does not have estrogen receptors, progesterone receptors, or HER2 protein. It tends to be more aggressive and challenging to treat. |
| What are the side effects of breast cancer treatment? | Side effects vary depending on the type of treatment but can include fatigue, nausea, hair loss, and lymphedema. |
| How can I support someone with breast cancer? | Offer practical help, listen to their concerns, and provide emotional support. |
| Where can I find more information and support? | Organizations like the American Cancer Society, National Breast Cancer Foundation, and Susan G. Komen provide valuable information and support resources. You can also find answers to your questions for free on WHAT.EDU.VN. |
| What are the latest advances in breast cancer research? | Research is ongoing in areas such as targeted therapies, immunotherapy, and early detection methods. |
13. The Importance of Support and Resources
Facing a breast cancer diagnosis can be overwhelming. Having access to support and resources is essential for coping with the emotional, physical, and financial challenges of the disease.
13.1. Support Groups
Support groups provide a safe and supportive environment for individuals with breast cancer to share their experiences and connect with others who understand what they are going through.
13.2. Counseling
Counseling can help individuals cope with the emotional impact of a breast cancer diagnosis and treatment.
13.3. Financial Assistance
Financial assistance programs can help individuals with the costs of treatment, transportation, and other expenses.
13.4. Educational Resources
Educational resources can provide individuals with information about breast cancer, treatment options, and coping strategies.
14. The Future of Breast Cancer Research
Ongoing research is leading to new advances in the prevention, detection, and treatment of breast cancer. Some promising areas of research include:
- Targeted Therapies: Developing drugs that target specific proteins or genes involved in cancer growth.
- Immunotherapy: Harnessing the power of the immune system to fight cancer.
- Early Detection Methods: Developing new methods for detecting breast cancer early, such as liquid biopsies and advanced imaging techniques.
- Personalized Medicine: Tailoring treatment to the individual characteristics of each patient’s cancer.
15. Call to Action: Get Your Questions Answered on WHAT.EDU.VN
Navigating the complexities of breast cancer can be challenging, but you don’t have to do it alone. At WHAT.EDU.VN, we understand that you might have many questions and concerns. Our platform provides a free and accessible resource to get your questions answered quickly and accurately. Whether you’re looking for information on symptoms, diagnosis, treatment options, or simply need guidance on where to turn for support, we’re here to help.
Don’t let uncertainty hold you back. Visit WHAT.EDU.VN today to ask your questions and connect with a community of knowledgeable individuals. Our team is dedicated to providing you with the information you need to make informed decisions about your health.
Address: 888 Question City Plaza, Seattle, WA 98101, United States
Whatsapp: +1 (206) 555-7890
Website: what.edu.vn
Take control of your health journey and empower yourself with knowledge. Your questions matter, and we’re here to provide the answers.