Opioid addiction is a significant public health concern, affecting millions worldwide. Medication-Assisted Treatment (MAT) has emerged as a cornerstone in combating this crisis, offering a comprehensive approach that combines medication with counseling and behavioral therapies. Among the medications used in MAT, buprenorphine stands out as a vital tool in helping individuals overcome opioid dependence. But What Is Buprenorphine, and how does it work?
Buprenorphine is a prescription medication approved by the Food and Drug Administration (FDA) in October 2002 for the treatment of opioid use disorder (OUD). It is categorized as a partial opioid agonist, and its unique pharmacological properties make it an effective and safer alternative to full opioid agonists like heroin or morphine. Buprenorphine treatment, when coupled with therapy and support systems, provides a holistic strategy to manage opioid dependency and facilitate recovery.
How Does Buprenorphine Work in the Body?
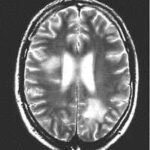
Understanding what buprenorphine is also involves knowing its mechanism of action. Buprenorphine works by interacting with opioid receptors in the brain, specifically the mu opioid receptor and the kappa receptor. It acts as a partial agonist at the mu receptor, meaning it activates this receptor but to a lesser degree than full agonists like heroin or prescription pain pills. Simultaneously, it functions as an antagonist at the kappa receptor.
This unique dual action is key to buprenorphine’s therapeutic benefits:
- Displacement of Full Opioid Agonists: Buprenorphine has a high affinity for the mu opioid receptor. This means it can effectively displace other opioids, such as heroin, methadone, and morphine, from these receptors. By doing so, it reduces the euphoric effects of these full agonists and blocks the rewarding sensations that contribute to addiction.
- Reduced Withdrawal Symptoms and Cravings: As a partial agonist, buprenorphine provides enough opioid effect to reduce withdrawal symptoms and cravings associated with opioid dependence. This helps individuals transition away from illicit or misused opioids more comfortably.
- Ceiling Effect and Overdose Safety: Unlike full opioid agonists, buprenorphine exhibits a “ceiling effect.” This means that beyond a certain dose, increasing the amount of buprenorphine does not lead to a proportional increase in opioid effects. This ceiling effect is a critical safety feature, significantly reducing the risk of respiratory depression, the primary cause of death in opioid overdose, compared to full opioid agonists.
- Lower Abuse Potential: Due to its partial agonist properties and ceiling effect, buprenorphine has a lower potential for misuse compared to full opioid agonists. This makes it a safer option for outpatient treatment settings.
What are the Benefits of Buprenorphine Treatment for Opioid Dependence?
Buprenorphine offers several significant advantages in the treatment of opioid dependence, making it a preferred choice for many patients and healthcare providers. These benefits include:
- Reduced Risk of Misuse and Diversion: The partial agonist nature and ceiling effect of buprenorphine contribute to a lower risk of misuse compared to full agonists. Furthermore, many buprenorphine products are combined with naloxone, an opioid antagonist. Naloxone has poor oral bioavailability, meaning it has little effect when taken sublingually as directed. However, if someone attempts to inject the buprenorphine/naloxone combination, the naloxone will precipitate withdrawal symptoms, deterring misuse via injection.
- Less Severe Withdrawal Symptoms: While buprenorphine can cause withdrawal if abruptly discontinued, the withdrawal symptoms are generally milder and shorter in duration compared to those associated with full opioid agonists. This facilitates easier discontinuation of the medication when appropriate.
- Greater Safety in Overdose Situations: The ceiling effect of buprenorphine significantly reduces the risk of fatal respiratory depression in overdose compared to full opioid agonists like heroin or methadone.
- Increased Accessibility to Treatment: A major advantage of buprenorphine is its accessibility. Unlike methadone, which in the US is primarily dispensed through highly regulated opioid treatment programs (OTPs), buprenorphine can be prescribed and dispensed in physician offices, community hospitals, health departments, and correctional facilities. This expanded access, enabled by the Drug Addiction Treatment Act of 2000 (DATA 2000), allows more individuals to receive timely and effective treatment for opioid dependence.
- “Feeling Normal” Effect: Buprenorphine provides enough opioid agonist effect to help patients “feel normal,” reducing cravings and withdrawal symptoms without causing significant euphoria or sedation when taken as prescribed. This allows individuals to focus on their recovery and engage in daily life.
Different Forms and Brands of Buprenorphine
Buprenorphine is available in various formulations and brand names, each designed for specific routes of administration and treatment needs. FDA-approved buprenorphine products for opioid dependency include:
- Suboxone: A combination of buprenorphine and naloxone, available as a sublingual film. It is one of the most commonly prescribed brands and is designed to deter misuse.
- Zubsolv: Another buprenorphine and naloxone combination product, available as sublingual tablets. Zubsolv is formulated to dissolve faster than some other sublingual tablets.
- Bunavail: A buprenorphine and naloxone combination administered as a buccal film that adheres to the inside of the cheek.
- Buprenorphine (transmucosal products): This category refers to various generic and brand-name buprenorphine products available in transmucosal forms (films or tablets) for the treatment of opioid dependency.
- Buprenex: An injectable form of buprenorphine primarily used for pain management, but not typically used for opioid dependence treatment in outpatient settings.
What are the Potential Side Effects of Buprenorphine?
Like all medications, buprenorphine can cause side effects. Common side effects are generally similar to those associated with opioids, although often milder due to its partial agonist nature. These can include:
- Nausea and vomiting
- Constipation
- Muscle aches and cramps
- Insomnia (difficulty sleeping)
- Cravings for opioids
- Distress and irritability
- Fever
- Headache
- Sweating
It’s crucial to discuss any side effects with a healthcare provider. Many side effects are manageable, and some may subside over time as the body adjusts to the medication.
Understanding Buprenorphine Misuse Potential and Safety Precautions
While buprenorphine has a lower misuse potential than full opioid agonists, it’s not without risk. Misuse can occur, particularly among individuals without opioid dependence who seek to experience euphoric effects, especially if injected. The combination with naloxone in products like Suboxone is designed to mitigate this risk.
To ensure safe use of buprenorphine, individuals should adhere to the following precautions:
- Strictly follow prescribed dosage and administration instructions.
- Avoid taking other medications, including over-the-counter drugs and herbal supplements, without consulting a doctor. Drug interactions can occur and may be dangerous.
- Do not use illicit drugs, drink alcohol, or take sedatives, tranquilizers, or other central nervous system depressants while taking buprenorphine. Combining these substances can increase the risk of respiratory depression and overdose.
- Inform your doctor about any pre-existing liver conditions. Buprenorphine is metabolized by the liver, and liver impairment may affect its processing in the body.
Buprenorphine Use During Pregnancy and Breastfeeding
The use of buprenorphine during pregnancy and breastfeeding requires careful consideration. Limited data exists on the effects of buprenorphine on pregnant women with opioid dependence and their babies. However, available case reports have not indicated major adverse outcomes associated with buprenorphine use during pregnancy. The FDA classifies buprenorphine as a Pregnancy Category C medication, meaning animal studies have shown adverse effects, but there are no adequate studies in humans, or human studies are lacking.
Methadone remains the established standard of care for MAT in pregnant women with opioid dependence in the United States. However, buprenorphine is increasingly being used and studied as an alternative. Women who are pregnant or breastfeeding and struggling with opioid dependence should have a detailed discussion with their healthcare provider to determine the safest and most appropriate treatment plan for themselves and their babies.
The Three Phases of Buprenorphine Treatment for Opioid Dependence
Buprenorphine treatment for opioid dependence typically involves three distinct phases:
- Induction Phase: This is the initiation phase, where buprenorphine treatment is started under medical supervision. It usually takes place in a qualified physician’s office or certified OTP. Buprenorphine is administered when the individual has been abstinent from opioids for 12-24 hours and is experiencing early withdrawal symptoms. It’s crucial that the patient is in the early stages of withdrawal to prevent precipitated withdrawal, which can occur if buprenorphine is given when other opioids are still active in the system.
- Stabilization Phase: Once the patient is inducted, the stabilization phase begins. During this phase, the buprenorphine dose is adjusted to minimize or eliminate withdrawal symptoms, suppress cravings, and reduce side effects. The goal is for the patient to discontinue or significantly reduce their use of problem opioids and experience minimal disruptions to their daily life.
- Maintenance Phase: In the maintenance phase, the patient is stable on a steady dose of buprenorphine. The duration of this phase is individualized and can be long-term, even indefinite, depending on the patient’s needs and progress. For some patients, medically supervised withdrawal from buprenorphine may be considered after stabilization, followed by continued therapy and support to prevent relapse.
Throughout all phases of buprenorphine treatment, counseling, behavioral therapies, and participation in social support programs are crucial components of a comprehensive recovery plan.
Buprenorphine Versus Methadone: Key Differences
Buprenorphine and methadone are both effective medications for opioid dependence, but they have key differences. Methadone is a full opioid agonist, while buprenorphine is a partial agonist. Methadone is typically dispensed daily at specialized OTPs, offering a highly structured treatment environment. Buprenorphine, with its increased accessibility and lower risk profile, can be prescribed in more flexible settings.
Studies suggest that buprenorphine is as effective as moderate doses of methadone. However, for individuals with high levels of physical dependence on opioids, higher doses of methadone may be more effective in suppressing cravings and preventing relapse. The choice between buprenorphine and methadone should be made in consultation with a healthcare provider, considering individual patient needs, preferences, and the severity of their opioid dependence.
Conclusion: Buprenorphine as a Vital Tool in Opioid Addiction Treatment
What is buprenorphine? It is a groundbreaking medication that has revolutionized the treatment of opioid dependence. As a partial opioid agonist, buprenorphine offers a unique combination of effectiveness and safety, reducing withdrawal symptoms and cravings while minimizing the risks of misuse and overdose. Its accessibility, various formulations, and integration within comprehensive MAT programs make it a crucial tool in helping individuals reclaim their lives from opioid addiction and achieve long-term recovery. If you or someone you know is struggling with opioid dependence, exploring buprenorphine treatment options with a healthcare professional is a vital first step towards healing and hope.