A CO2 blood test, often referred to as a bicarbonate test, is a crucial diagnostic tool that measures the amount of carbon dioxide in your blood. But why is carbon dioxide important, and what does it tell us about our health? Carbon dioxide, in the form of bicarbonate, is a natural waste product produced by your body as it converts food into energy. Bicarbonate is also a vital electrolyte, playing a key role in maintaining your body’s hydration levels and ensuring the correct acid-base balance in your blood. This balance, also known as pH balance, is essential for all bodily functions to operate correctly. When the levels of bicarbonate in your blood are either too high or too low, it can indicate underlying health issues, ranging from digestive problems to kidney or liver conditions.
Alt text: A medical professional drawing blood from a patient’s arm for a blood test, highlighting the common procedure for CO2 blood tests.
Delving Deeper: The Role of Bicarbonate and CO2 in Your Body
To understand the CO2 blood test, it’s helpful to grasp the relationship between bicarbonate and carbon dioxide within your body. When carbon dioxide is produced as a waste product, much of it is transported in your blood as bicarbonate ions. This conversion is essential because bicarbonate acts as a buffer, helping to regulate the pH of your blood. Think of it as a natural balancing system, ensuring your blood isn’t too acidic or too alkaline. This delicate balance is critical for the proper functioning of your organs and cells. Electrolytes like bicarbonate are crucial for nerve and muscle function, hydration, and maintaining stable blood pressure. Therefore, a CO2 blood test isn’t just measuring waste; it’s assessing a vital component of your body’s regulatory system.
Why Your Doctor Might Order a CO2 Blood Test
A CO2 blood test is often part of a broader electrolyte panel, which also measures sodium, potassium, and chloride levels. Doctors frequently include this test in routine check-ups to get a general overview of your health. However, it becomes particularly important when you’re experiencing certain symptoms or if your doctor suspects specific medical conditions.
Your doctor may specifically order a CO2 blood test if you are experiencing:
- Persistent Vomiting or Diarrhea: These conditions can disrupt your electrolyte balance, including bicarbonate levels.
- Breathing Difficulties: Abnormal CO2 levels can be both a cause and a consequence of respiratory problems.
- Unexplained Weakness or Fatigue: Electrolyte imbalances can lead to feelings of weakness and tiredness.
Furthermore, if you are already undergoing treatment for conditions affecting your kidneys, liver, lungs, or digestive system, your doctor may use regular CO2 blood tests to monitor the effectiveness of your treatment plan and medication. These tests help ensure that your body’s delicate balance is being maintained throughout your medical care.
Alt text: A doctor discussing blood test results with a patient, emphasizing the importance of communication and understanding CO2 levels in healthcare.
What to Expect During a CO2 Blood Test
The CO2 blood test is a standard and straightforward procedure. It’s typically performed by a doctor or nurse who will collect a blood sample from a vein in your arm using a needle. The process is quick, and while you might feel a brief sting when the needle is inserted, it’s generally not painful.
Before the test, it’s important to inform your doctor about any medications or supplements you are currently taking. Certain substances can influence your blood test results. Even some foods, like grapefruit and tangerines due to their acidity, might potentially affect the outcome. Your healthcare provider will give you specific instructions if any preparation is needed.
The blood sample collected is then sent to a laboratory for analysis. The lab technicians will separate the fluid portion of your blood (serum or plasma) from the blood cells and platelets. To measure bicarbonate levels, they add acid to the fluid, which releases carbon dioxide from the bicarbonate. The change in acidity of the sample is then measured to determine the amount of bicarbonate present.
Interpreting Your CO2 Blood Test Results: What Do High and Low Levels Mean?
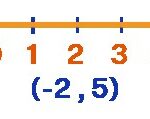
The results of your CO2 blood test are typically reported in millimoles per liter of fluid (mmol/L). The normal range for adults generally falls between 23 and 29 mmol/L, but it’s important to note that these ranges can slightly vary between different laboratories. Your lab report will usually provide the specific normal range they use for comparison.
Low CO2 Levels (Low Bicarbonate)
A lower than normal CO2 level can indicate a condition called metabolic acidosis, where there is too much acid in your body fluids. This can be caused by several factors, including:
- Kidney Disease: Impaired kidney function can lead to acid buildup.
- Diabetic Ketoacidosis: A serious complication of diabetes where the body produces excess acids due to insufficient insulin.
- Metabolic Acidosis: Various conditions that cause an overproduction of acid or prevent the kidneys from removing enough acid.
- Addison’s Disease: A rare disorder affecting the adrenal glands and hormone production.
- Ethylene Glycol Poisoning: Ingestion of antifreeze and certain household products.
- Aspirin Overdose: Excessive intake of aspirin can lead to acidosis.
High CO2 Levels (High Bicarbonate)
Conversely, a higher than normal CO2 level can suggest metabolic alkalosis, indicating an excess of base (alkali) in your body fluids. This can be associated with:
- Severe Vomiting: Loss of stomach acid can lead to alkalosis.
- Certain Diuretics: Some medications can cause the kidneys to remove too much acid.
- Endocrine Disorders: Conditions affecting hormone production.
It’s crucial to remember that CO2 blood test results are just one piece of the puzzle. Your doctor will consider your results in conjunction with your symptoms, medical history, and other test findings to reach an accurate diagnosis and recommend the appropriate course of action. If your CO2 levels are outside the normal range, it doesn’t automatically mean you have a serious medical condition, but it does warrant further investigation and discussion with your healthcare provider.