Are you curious about the science of blood and its disorders? WHAT.EDU.VN offers a free platform to explore the world of hematology and find answers to all your questions. Dive in to understand blood, blood-forming organs, and related diseases, and let us help you learn more. Discover insights into hematological testing and its importance.
1. What Is Hematology? An Overview of Blood Science
Hematology is the branch of medicine dedicated to the study of blood, the organs that produce blood (like bone marrow), and diseases related to blood. The term “heme” comes from the Greek word for blood. Hematology is essential for diagnosing and treating a wide range of conditions, from common anemias to complex blood cancers. This field uses various laboratory tests and clinical evaluations to understand and manage blood-related issues. Hematological tests play a crucial role in detecting and diagnosing various diseases, including hemophilia, anemia, leukemia, sickle cell anemia, lymphomas, and several infections.
.jpg)
2. What Are the Main Areas of Focus in Hematology?
Hematology focuses on several key areas:
- Blood Cell Production: Understanding how blood cells (red cells, white cells, and platelets) are formed in the bone marrow.
- Blood Disorders: Diagnosing and managing diseases like anemia, leukemia, and clotting disorders.
- Blood Transfusions: Ensuring safe and effective blood transfusions for patients who need them.
- Coagulation: Studying the mechanisms of blood clotting and related disorders such as hemophilia and thrombosis.
- Hematological Malignancies: Treating cancers of the blood and bone marrow, including leukemia, lymphoma, and myeloma.
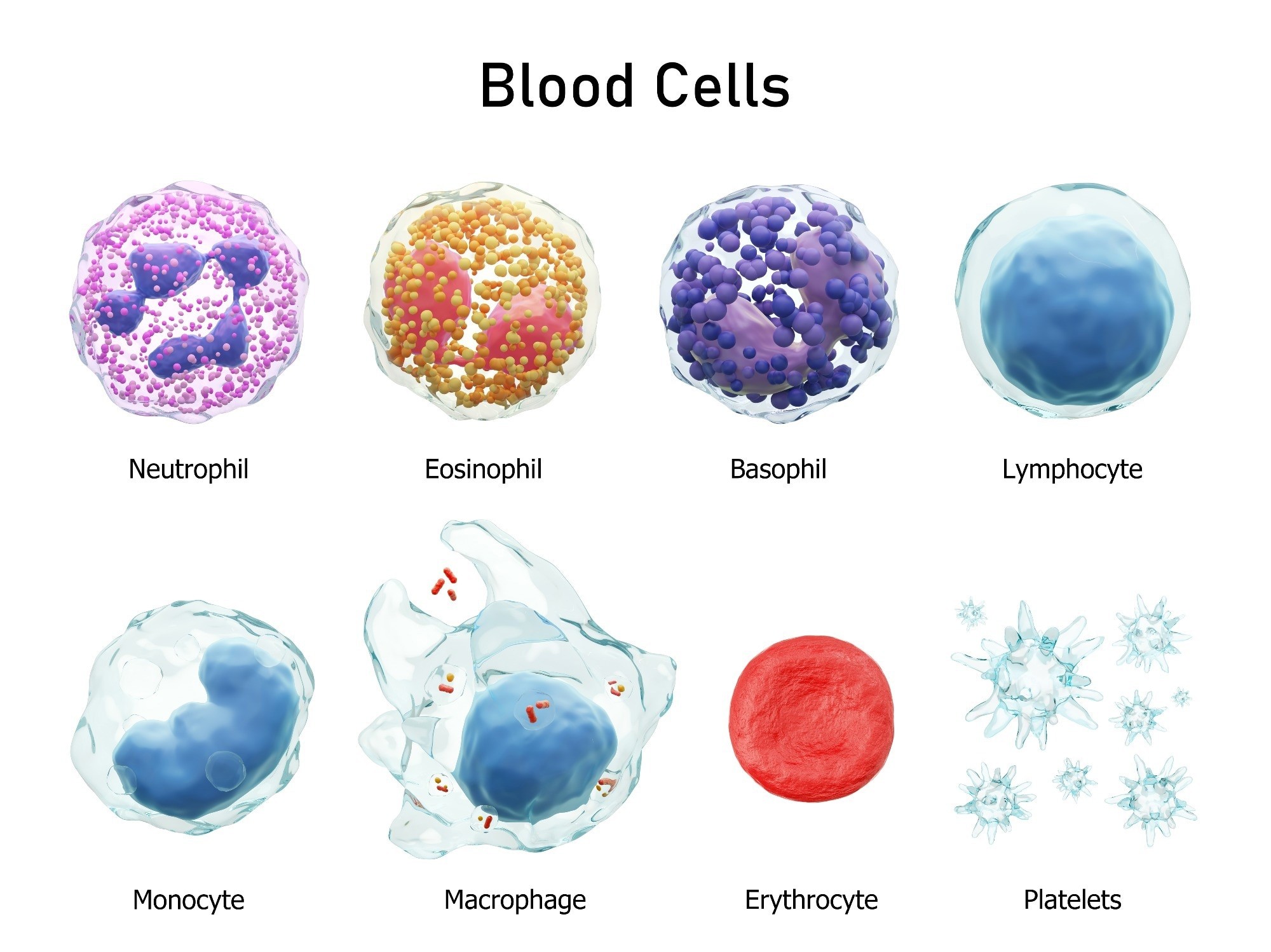
3. What Are the Different Types of Blood Cells and Their Functions?
Blood consists of three main types of cells, each with specific functions:
| Cell Type | Function |
|---|---|
| Red Blood Cells | Carry oxygen from the lungs to the rest of the body. They contain hemoglobin, a protein that binds to oxygen. |
| White Blood Cells | Fight infections and play a role in the immune system. There are different types of white blood cells, each targeting specific threats. |
| Platelets | Help in blood clotting by clumping together to form a plug that stops bleeding. They are essential for wound healing and preventing excessive blood loss. |
4. What Are Common Hematological Diseases and Disorders?
Hematological disorders include a wide range of conditions affecting the blood and blood-forming organs. These disorders can be classified into malignant and nonmalignant blood disorders. Nonmalignant blood disorders include hemoglobinopathies such as thalassemia and sickle-cell anemia, other types of anemias, and coagulopathies such as hemophilia. Hemoglobinopathies are genetic diseases and, apart from α- and β-thalassemia, include diseases caused by abnormal hemoglobin structure, manifesting in mild to severe anemia and multi-organ problems. Clotting disorders with genetic causes also include hemophilia and Von Willebrand disease, both of which are caused by low levels of clotting factors in the blood.
Other nonmalignant disorders like anemia and pulmonary embolism could be caused by various factors, including diet and lifestyle. Idiopathic thrombocytopenic purpura is a hematological disease characterized by an abnormal drop in the blood platelet concentration, which then results in bruising, nosebleeds, bleeding gums, and internal bleeding since platelets are involved in clotting. While idiopathic thrombocytopenic purpura is not inherited or contagious, the cause is yet unknown. In most cases, idiopathic thrombocytopenic purpura occurs in children after a viral infection such as chicken pox.
Malignant blood disorders include leukemia, lymphomas, and myelomas and can affect people of all ages. Malignant hematological disorders could be caused by various factors, including genetics, lifestyle, and environment. Polycythemia vera is a form of leukemia known as a myeloproliferative neoplasm, characterized by excessive production of red blood cells in the bone marrow, which causes blood to become more viscous and increases the risks of clots and heart attack. Myelofibrosis is another myeloproliferative form of leukemia where the bone marrow produces an excess of stem cells resulting in inflammation and scar tissue formation in the bone marrow. Malignant lymphomas, including Hodgkin’s lymphoma, affect the lymphatic system and result in abnormal lymphocytes.
Myelodysplastic syndromes refer to a group of cancers where blood stem cells in the bone marrow fail to mature and form various mature blood cells. This results in refractory anemia, refractory cytopenia, chronic myelomonocytic leukemia, and various other cancers due to the insufficiency of red and white blood cells in the blood. Multiple myeloma is a form of cancer that results in excess plasma cells in the blood. The overcrowding of plasma cells in the blood causes a shortage of red blood cells, platelets, and white blood cells resulting in anemia, thrombocytopenia, and leukopenia, respectively. Multiple myeloma can also affect the osteoblasts and osteoclasts that keep bones healthy, causing bone degeneration and fractures.
- Anemia: A condition characterized by a deficiency of red blood cells or hemoglobin in the blood, resulting in fatigue and weakness.
- Leukemia: A type of cancer that affects the blood and bone marrow, characterized by an abnormal increase in white blood cells.
- Lymphoma: Cancer that begins in the lymphatic system, affecting the cells that help fight infection.
- Myeloma: A cancer of plasma cells, a type of white blood cell that produces antibodies.
- Hemophilia: A genetic disorder that impairs the body’s ability to make blood clots, leading to excessive bleeding.
- Thrombosis: The formation of a blood clot inside a blood vessel, obstructing the flow of blood.
- Thrombocytopenia: A condition characterized by a low platelet count, leading to easy bruising and bleeding.
5. How Is Anemia Diagnosed and Treated?
Anemia is typically diagnosed through a complete blood count (CBC), which measures the levels of red blood cells, hemoglobin, and other related parameters. Further tests may be needed to determine the underlying cause of anemia, such as iron deficiency, vitamin deficiency, or chronic disease.
Treatment for anemia depends on the cause:
- Iron Deficiency Anemia: Iron supplements and dietary changes to increase iron intake.
- Vitamin Deficiency Anemia: Vitamin B12 or folate supplements.
- Anemia of Chronic Disease: Managing the underlying condition causing the anemia.
- Aplastic Anemia: Blood transfusions, bone marrow transplant, or medications to stimulate blood cell production.
6. What Are the Symptoms and Treatment Options for Leukemia?
Leukemia symptoms vary depending on the type and stage of the disease, but common symptoms include:
- Fatigue and weakness
- Frequent infections
- Easy bleeding or bruising
- Bone pain
- Swollen lymph nodes
Treatment options for leukemia include:
- Chemotherapy: Using drugs to kill cancer cells.
- Radiation Therapy: Using high-energy rays to damage cancer cells.
- Stem Cell Transplant: Replacing damaged bone marrow with healthy stem cells.
- Targeted Therapy: Using drugs that target specific abnormalities in cancer cells.
- Immunotherapy: Using the body’s own immune system to fight cancer.
7. What Is the Role of Blood Transfusions in Hematology?
Blood transfusions are a critical part of hematology, used to replace blood components lost due to injury, surgery, or disease. Transfusions can involve:
- Red Blood Cells: To treat anemia and improve oxygen delivery.
- Platelets: To control bleeding in patients with thrombocytopenia.
- Plasma: To provide clotting factors in patients with bleeding disorders.
- White Blood Cells: Rarely used, but can help fight severe infections in patients with low white blood cell counts.
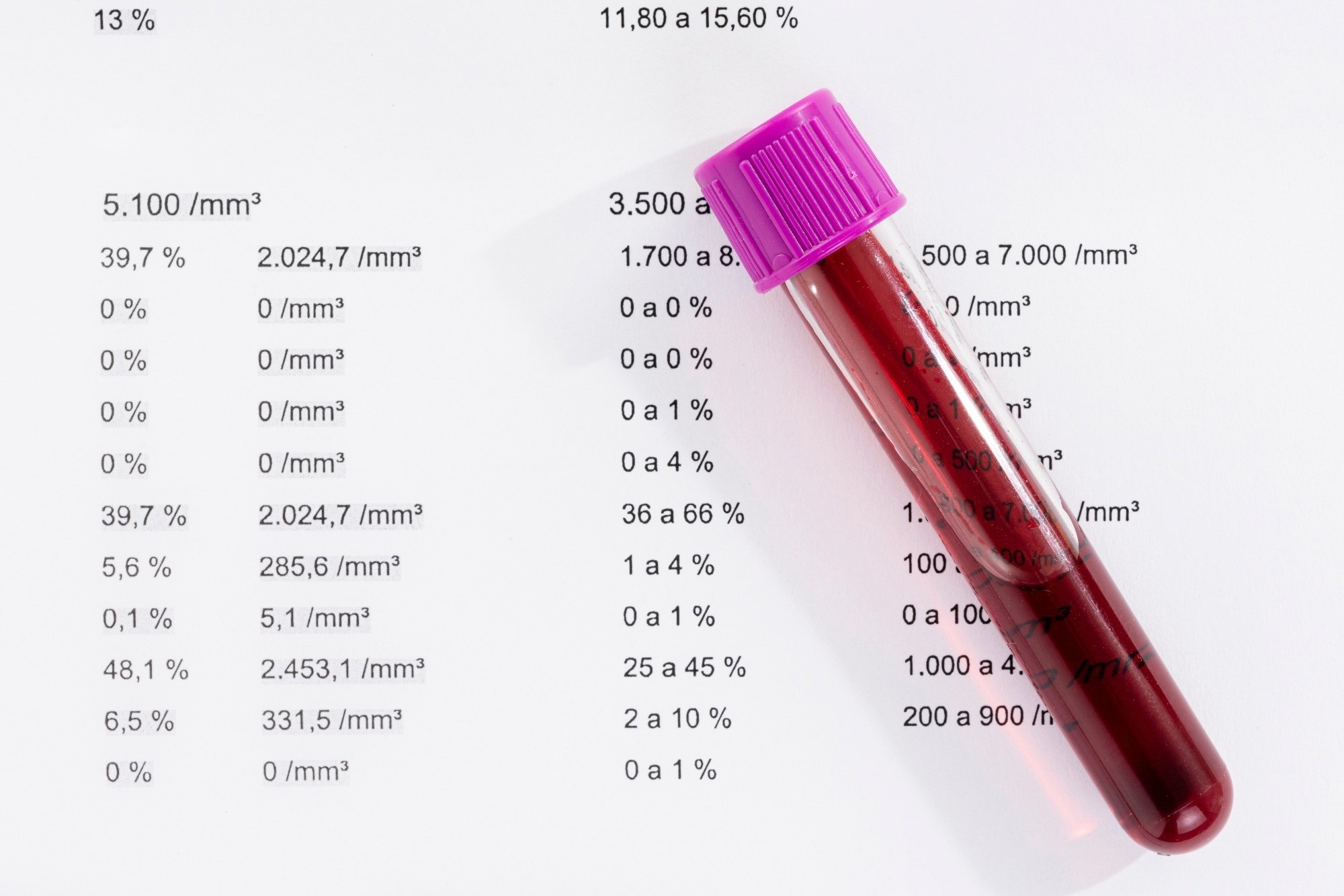
8. What Are the Common Tests Used in Hematology?
Blood tests provide valuable information for diagnosing hematological and non-hematological diseases and disorders. A complete blood count (CBC) is one of the most common blood tests employed in disease diagnosis. The hematological parameters measured in a CBC include the number of white and red blood cells, platelet count, hematocrit red blood cell volume, hemoglobin concentration, differential white blood count, and various other red blood cell indices. Complete blood counts are used in diagnosing infections, anemia, blood-related cancers, and inflammatory diseases.
Platelet counts are informative about bleeding and clotting disorders. Clotting-related disorders such as hemophilia can also be monitored and diagnosed using coagulant tests such as prothrombin time and partial thromboplastin time. These tests can also be used to monitor anticoagulation or anticlotting therapies.
The bone marrow test is one of the rarer hematological tests and involves analyzing cells from the bone marrow to diagnose diseases such as multiple myelomas.
Common hematology tests include:
- Complete Blood Count (CBC): Measures the levels of red blood cells, white blood cells, and platelets.
- Blood Smear: Examines blood cells under a microscope to identify abnormalities.
- Coagulation Tests: Assess the blood’s ability to clot properly.
- Bone Marrow Biopsy: Removes a sample of bone marrow for examination, used to diagnose blood cancers and other disorders.
- Flow Cytometry: Identifies specific cells and their characteristics, often used in diagnosing leukemia and lymphoma.
9. How Does Hematology Relate to Oncology?
Hematology and oncology are closely related, with many specialists trained in both fields (hematologist-oncologists). Hematology focuses on blood disorders, while oncology focuses on cancer. However, many hematological disorders, such as leukemia and lymphoma, are cancers, requiring both hematological and oncological expertise.
Hematologist-oncologists are specialists who do not perform cancer-related surgeries but treat the conditions with medications. In addition, they provide cancer screening tests, monitor chemotherapy regimens, and work with other specialists such as oncology surgeons, pathologists, and radiation oncologists.
10. What Is the Role of a Hematologist?
Hematology is practiced by hematologists and hematopathologists. Hematologists are medical doctors with additional years of training in hematology. They are involved in direct patient care and diagnose and manage various hematological diseases, including cancers of the blood and bone marrow. Hematopathologists are medical doctors with board certifications in clinical and anatomical pathology. They study not only blood and blood-related diseases but also the tissues and organs, such as the spleen, lymph nodes, and the thymus, that use blood for their physiological functions. Hematopathologists diagnose blood and lymph-related conditions using tissue and blood samples in the laboratory.
Hematologists specializing in nonmalignant blood disorders use various blood smears, tests, and molecular diagnostic tools to formulate a proper diagnosis and treatment plan for their patients. They are sometimes also involved in the long-term care of patients with chronic hematological diseases.
Specialists in malignant hematological disorders also require broad knowledge in other fields, such as infectious diseases. They can further specialize in treatment methods such as bone marrow transplants, used for many blood cancers. Transfusion medicine is yet another area of specialization in treating malignant hematological disorders.
Since blood is the human body’s life force, almost all aspects of human health are linked to the circulatory system. Hematologists can collaborate with specialists from many other disciplines, such as surgeons, cardiologists, immunologists, and infectious disease specialists. They can also serve as consultants in other medical fields, such as trauma, neurosurgery, and cardiovascular diseases.
Hematologists are medical doctors specializing in the diagnosis, treatment, and prevention of blood disorders and cancers. Their roles include:
- Diagnosing blood disorders through physical exams, blood tests, and bone marrow biopsies.
- Developing treatment plans tailored to each patient’s specific condition.
- Managing and monitoring patients undergoing treatment, such as chemotherapy or blood transfusions.
- Providing long-term care and support for patients with chronic blood disorders.
- Conducting research to improve understanding and treatment of blood diseases.
11. What Training Is Required to Become a Hematologist?
Hematologists are required to complete a four-year medical degree, followed by three or four years of residency in internal medicine or internal medicine and pediatrics combined. After that, they spend two or three more years learning to diagnose and treat blood disorders. Hematology specialization is often combined with a specialization in oncology. Hematopathologists are required to first complete a residency in pathology before specializing in hematology.
Extensive first-hand practical experience in a recognized training center provides hematologists with expertise in diagnosing the cause of abnormalities in blood formation and other blood disorders and cancers using laboratory tests and in treating patients with hematological diseases.
To become a hematologist, one must complete:
- A four-year bachelor’s degree
- Four years of medical school to earn a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree
- A three-year residency in internal medicine or pediatrics
- A two- to three-year fellowship in hematology
What is a Haematologist?
12. What Is the Difference Between a Hematologist and a Hematopathologist?
While both hematologists and hematopathologists focus on blood disorders, their roles differ:
- Hematologist: Primarily involved in direct patient care, diagnosing and managing blood disorders and cancers.
- Hematopathologist: Focuses on the laboratory diagnosis of blood diseases, analyzing blood and bone marrow samples to identify abnormalities.
Hematopathologists are medical doctors with board certifications in clinical and anatomical pathology. They study not only blood and blood-related diseases but also the tissues and organs, such as the spleen, lymph nodes, and the thymus, that use blood for their physiological functions. Hematopathologists diagnose blood and lymph-related conditions using tissue and blood samples in the laboratory.
13. How Does Hematology Contribute to Medical Research?
Hematology plays a vital role in medical research, contributing to:
- Developing new diagnostic tools and treatments for blood disorders and cancers.
- Understanding the genetic and molecular basis of blood diseases.
- Improving the safety and effectiveness of blood transfusions.
- Finding new ways to prevent blood clots and bleeding disorders.
- Advancing stem cell transplantation techniques.
14. What Are Some Recent Advances in Hematology?
Recent advances in hematology include:
- Targeted Therapies: Drugs that specifically target cancer cells, reducing side effects.
- Immunotherapies: Treatments that harness the body’s immune system to fight cancer.
- Gene Therapies: Correcting genetic defects that cause blood disorders.
- Improved Stem Cell Transplantation: Enhancing the safety and effectiveness of bone marrow transplants.
- Better Diagnostic Tools: More sensitive and accurate tests for detecting blood diseases.
15. How Is Hematology Involved in Treating Bleeding Disorders Like Hemophilia?
Hematology is crucial in managing bleeding disorders like hemophilia, which is a genetic condition characterized by the body’s inability to form blood clots properly. The hematologist’s role includes:
- Diagnosis: Identifying the specific type and severity of hemophilia through blood tests.
- Treatment: Providing replacement therapy with clotting factors to prevent and control bleeding episodes.
- Monitoring: Regularly assessing the patient’s clotting factor levels and adjusting treatment as needed.
- Education: Educating patients and families about managing the condition and preventing complications.
- Comprehensive Care: Coordinating care with other specialists, such as physical therapists and orthopedic surgeons, to address the long-term effects of hemophilia.
16. What Is the Significance of Hematology in Bone Marrow Transplantation?
Hematology is central to bone marrow transplantation, a procedure used to treat various blood cancers and disorders. The hematologist’s involvement includes:
- Patient Evaluation: Determining if a patient is a suitable candidate for bone marrow transplantation.
- Donor Matching: Finding a matching donor, either a related or unrelated individual, whose bone marrow is compatible with the patient.
- Conditioning Regimen: Administering chemotherapy and/or radiation therapy to prepare the patient’s body for the transplant.
- Transplantation: Infusing the donor’s stem cells into the patient’s bloodstream.
- Post-Transplant Care: Managing complications, such as infections and graft-versus-host disease, and providing long-term follow-up care.
17. How Can Diet and Lifestyle Affect Blood Health?
Diet and lifestyle can significantly impact blood health:
- Iron-Rich Foods: Consuming foods rich in iron, such as leafy greens, red meat, and beans, can prevent iron deficiency anemia.
- Vitamin B12 and Folate: Ensuring adequate intake of vitamin B12 and folate, found in foods like eggs, dairy, and fortified grains, is essential for red blood cell production.
- Hydration: Staying hydrated helps maintain blood volume and prevents blood clots.
- Regular Exercise: Regular physical activity improves blood circulation and overall blood health.
- Avoiding Smoking: Smoking damages blood vessels and increases the risk of blood clots and other blood disorders.
- Limiting Alcohol: Excessive alcohol consumption can lead to anemia and other blood-related problems.
18. What Is the Role of Hematology in Autoimmune Disorders?
Hematology plays a role in managing autoimmune disorders that affect the blood, such as:
- Autoimmune Hemolytic Anemia: Where the body’s immune system destroys red blood cells.
- Immune Thrombocytopenic Purpura (ITP): Where the immune system attacks platelets, leading to bleeding problems.
Hematologists help diagnose these conditions and develop treatment plans to suppress the immune system and prevent further damage to blood cells. Treatments may include corticosteroids, intravenous immunoglobulin (IVIG), and other immunosuppressive drugs.
19. How Does Hematology Address Blood Clotting Disorders?
Hematology is crucial in diagnosing and managing blood clotting disorders, which can lead to either excessive bleeding or excessive clotting. Common conditions include:
- Deep Vein Thrombosis (DVT): Blood clots in the deep veins, usually in the legs.
- Pulmonary Embolism (PE): Blood clots that travel to the lungs.
- Thrombophilia: Genetic disorders that increase the risk of blood clots.
Hematologists use blood tests to assess clotting function and develop treatment plans to prevent and manage blood clots. Treatments may include anticoagulants (blood thinners), thrombolytic therapy (clot-busting drugs), and lifestyle changes to reduce the risk of clotting.
20. What Are the Ethical Considerations in Hematology?
Ethical considerations in hematology include:
- Informed Consent: Ensuring patients understand the risks and benefits of treatments and make informed decisions.
- Confidentiality: Protecting patient privacy and medical information.
- Access to Care: Ensuring equitable access to hematological services, regardless of socioeconomic status.
- Research Ethics: Conducting research in a responsible and ethical manner, protecting the rights and welfare of research participants.
- End-of-Life Care: Providing compassionate and supportive care for patients with terminal blood disorders, respecting their wishes and values.
21. How Is Hematology Involved in Global Health Initiatives?
Hematology plays a role in global health initiatives by:
- Addressing Anemia: Implementing programs to prevent and treat anemia in developing countries through iron supplementation and improved nutrition.
- Managing Hemoglobinopathies: Providing screening and treatment for genetic blood disorders like sickle cell anemia and thalassemia in affected populations.
- Improving Blood Transfusion Safety: Establishing safe blood transfusion practices to prevent the spread of infectious diseases.
- Training Healthcare Professionals: Educating and training healthcare professionals in hematology to improve the diagnosis and management of blood disorders in resource-limited settings.
- Conducting Research: Conducting research to understand the prevalence and impact of blood disorders in different regions and develop effective interventions.
22. What Are the Emerging Trends in Hematology?
Emerging trends in hematology include:
- Personalized Medicine: Tailoring treatments to individual patients based on their genetic and molecular profiles.
- Minimal Residual Disease (MRD) Testing: Using highly sensitive tests to detect small numbers of cancer cells after treatment, helping to predict relapse and guide further therapy.
- CAR-T Cell Therapy: Genetically modifying a patient’s own immune cells to target and destroy cancer cells, showing promising results in treating certain blood cancers.
- Liquid Biopsies: Analyzing blood samples to detect cancer DNA and other biomarkers, providing a non-invasive way to monitor disease progression and response to treatment.
- Artificial Intelligence (AI): Using AI to analyze large datasets and improve the accuracy and efficiency of hematological diagnoses.
23. How Can Patients Find Reliable Information About Hematological Conditions?
Patients can find reliable information about hematological conditions from:
- Healthcare Professionals: Consulting with hematologists, oncologists, and other healthcare providers.
- Reputable Websites: Visiting websites of medical organizations, such as the American Society of Hematology (ASH) and the Leukemia & Lymphoma Society (LLS).
- Patient Advocacy Groups: Contacting patient advocacy groups for support and resources.
- Medical Libraries: Accessing medical libraries and databases for peer-reviewed research articles.
- Educational Materials: Reviewing educational materials provided by healthcare organizations and patient advocacy groups.
24. What Support Services Are Available for Patients With Blood Disorders?
Support services available for patients with blood disorders include:
- Support Groups: Joining support groups to connect with other patients and share experiences.
- Counseling Services: Seeking counseling to cope with the emotional and psychological impact of blood disorders.
- Financial Assistance Programs: Applying for financial assistance to help with medical expenses.
- Educational Resources: Accessing educational resources to learn more about blood disorders and treatment options.
- Home Healthcare Services: Receiving home healthcare services to manage symptoms and treatment side effects.
25. What Is the Future of Hematology?
The future of hematology is promising, with ongoing research and innovation leading to:
- More Effective Treatments: Developing more effective and less toxic therapies for blood disorders and cancers.
- Personalized Approaches: Tailoring treatments to individual patients based on their unique characteristics.
- Early Detection: Improving early detection methods to diagnose blood disorders at an earlier stage, when they are more treatable.
- Prevention Strategies: Identifying and implementing strategies to prevent blood disorders, such as promoting healthy lifestyles and screening for genetic risk factors.
- Improved Quality of Life: Enhancing the quality of life for patients with blood disorders through better symptom management and supportive care.
Hematology is a dynamic and evolving field that plays a crucial role in improving the health and well-being of individuals affected by blood disorders. With ongoing research and innovation, the future of hematology holds great promise for more effective treatments, personalized approaches, and improved quality of life for patients with blood-related conditions.
Do you have more questions about hematology or any other topic? Don’t hesitate to ask on WHAT.EDU.VN and get free answers quickly.
Contact Us:
Address: 888 Question City Plaza, Seattle, WA 98101, United States
WhatsApp: +1 (206) 555-7890
Website: what.edu.vn
We are here to help you find the information you need.