Hemorrhoids, a surprisingly common ailment, affect millions of adults. By the age of 50, it’s estimated that about half of us will experience the discomfort of hemorrhoids, also known as piles. While rarely dangerous, these swollen veins in the rectum and anus can cause recurring pain, itching, and bleeding, significantly impacting daily life. Understanding what hemorrhoids are, what causes them, and the range of effective treatments available is key to managing and alleviating this condition. Let’s delve into the details of hemorrhoids and explore how to find relief.
Defining Hemorrhoids: More Than Just ‘Piles’
In reality, everyone is born with hemorrhoids. These aren’t inherently a disease, but rather normal anatomical structures. Hemorrhoids are essentially clusters of veins located beneath the mucous membranes lining the lower rectum and anus, acting like cushions to help control bowel movements. The term “hemorrhoids” in common usage, however, refers to the condition that develops when these veins become swollen and distended. Think of it similarly to varicose veins that can occur in the legs. This swelling and enlargement can lead to a variety of uncomfortable symptoms.
This condition arises because the blood vessels in the rectal and anal area are constantly working against gravity to return blood to the heart. This constant pressure, coupled with other factors, can lead to the veins becoming enlarged and problematic.
There are two main types of hemorrhoids, categorized by their location: internal and external.
Internal and external hemorrhoids 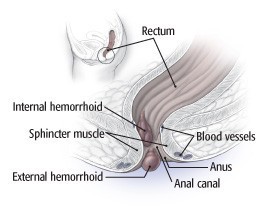 Diagram illustrating internal and external hemorrhoids
Diagram illustrating internal and external hemorrhoids
Alt text: Anatomical illustration comparing internal hemorrhoids located inside the rectum and external hemorrhoids situated outside the anus.
Types of Hemorrhoids: Internal vs. External
Understanding the distinction between internal and external hemorrhoids is important as their symptoms and treatment approaches can differ.
Internal Hemorrhoids
Internal hemorrhoids develop within the lower rectum and are typically not felt because they are located above the dentate line, where there are fewer nerve endings. The most common sign of internal hemorrhoids is painless rectal bleeding, often noticed as bright red blood on toilet paper or in the toilet bowl after a bowel movement.
Internal hemorrhoids can also prolapse, meaning they extend or protrude outside the anus. Prolapse can occur during bowel movements and may retract on their own or need to be gently pushed back in. Prolapsed hemorrhoids can cause discomfort and irritation, and may also collect mucus and stool particles, leading to anal itching, known as pruritus ani. The urge to scratch can exacerbate the problem.
External Hemorrhoids
External hemorrhoids, on the other hand, occur under the skin around the anus. Because they are located in an area with many nerve endings, external hemorrhoids are often more painful and uncomfortable than internal ones. The skin covering external hemorrhoids can become irritated, eroded, and itchy.
A particularly painful condition arises when a blood clot forms within an external hemorrhoid. This is known as a thrombosed external hemorrhoid. The pain can be sudden and severe, and you might feel a hard, tender lump around the anus. While the clot usually dissolves on its own, it can leave behind a skin tag – excess skin that may remain itchy or irritated.
What Causes Hemorrhoids? Unpacking the Root Causes
Several factors contribute to the development of hemorrhoids. Traditionally, they have been linked to factors that increase pressure on the veins in the rectum and anus.
-
Increased Pressure: Conditions that raise pressure in the lower rectum are major contributors. These include:
- Pregnancy: The growing uterus puts pressure on the veins in the pelvic area.
- Being Overweight or Obese: Excess weight adds pressure to these veins.
- Straining during Bowel Movements: This increases pressure in the anal canal.
-
Chronic Constipation: Constipation and the associated straining during bowel movements are long-standing associations with hemorrhoids. Straining interferes with blood flow, causing blood to pool and enlarge the veins.
-
Prolonged Sitting on the Toilet: Spending extended periods on the toilet can also contribute by increasing pressure and strain on the rectal veins.
-
Higher Resting Anal Canal Tone: Recent research suggests that individuals with hemorrhoids often have a naturally tighter anal canal, even when not straining. This increased muscle tone can contribute to pressure on the hemorrhoidal veins. Constipation further exacerbates this, as straining pushes hemorrhoids against this already tight sphincter muscle.
-
Weakening Connective Tissues: As we age, the tissues that support and hold hemorrhoids in place can weaken. This weakening can lead to hemorrhoids bulging and prolapsing more easily.
Symptoms of Hemorrhoids: Recognizing the Signs
The symptoms of hemorrhoids vary depending on whether they are internal or external. Common symptoms include:
- Rectal Bleeding: Bright red blood on toilet paper, in the toilet bowl, or on the stool. This is more typical of internal hemorrhoids.
- Rectal Pain or Discomfort: Pain can range from mild itching to severe pain, especially with external or thrombosed hemorrhoids.
- Itching in the Anal Area: Irritation and itching are common, particularly with prolapsed internal hemorrhoids or irritated external hemorrhoids.
- Prolapse: Protrusion of hemorrhoids outside the anus, usually associated with internal hemorrhoids.
- Lump Near the Anus: A tender lump can indicate a thrombosed external hemorrhoid.
- Fecal Leakage: In some cases, prolapsed internal hemorrhoids can cause minor fecal leakage.
It’s important to note that rectal bleeding can also be a symptom of other, more serious conditions, so it’s crucial to consult a doctor to determine the cause.
Diagnosing Hemorrhoids: When to See a Doctor
Often, hemorrhoids can be diagnosed with a simple medical history review and a physical examination. External hemorrhoids, especially thrombosed ones, are usually readily visible. A doctor may perform a digital rectal exam, inserting a gloved, lubricated finger into the rectum to feel for abnormalities and check for blood in the stool.
To further examine internal hemorrhoids and rule out other conditions, a doctor may use an anoscope. This is a short, rigid, tube-like instrument inserted into the rectum to visualize the anal canal.
If there is evidence of rectal bleeding or microscopic blood in the stool, especially in individuals over 45 or those with risk factors for colorectal cancer, further investigations may be recommended. These could include flexible sigmoidoscopy or colonoscopy. These procedures allow the doctor to examine the colon and rectum more thoroughly and rule out other causes of bleeding, such as polyps or cancer.
Hemorrhoid Treatment: From Home Remedies to Medical Procedures
Fortunately, many cases of hemorrhoids can be effectively managed, starting with conservative home treatments.
Home Remedies for Hemorrhoids: Self-Care Strategies
For mild to moderate hemorrhoid symptoms, home care strategies can provide significant relief. These remedies focus on softening stools, reducing straining, and soothing the irritated area.
-
Increase Fiber Intake: Dietary fiber is crucial for preventing and managing hemorrhoids. Fiber adds bulk to the stool, making it softer and easier to pass, thus reducing straining. Aim for 25-30 grams of fiber per day through fiber-rich foods like fruits, vegetables, whole grains, beans, and bran. Fiber supplements like psyllium husk (Metamucil) or methylcellulose (Citrucel) can also be helpful. Remember to increase fluid intake when increasing fiber to prevent constipation.
-
Stay Hydrated: Drinking plenty of water throughout the day helps keep stools soft and prevents constipation.
-
Regular Exercise: Moderate aerobic exercise, such as a 20-30 minute brisk walk daily, promotes regular bowel movements and overall health.
-
Don’t Delay Bowel Movements: When you feel the urge to go, go. Delaying bowel movements can lead to harder stools and increased straining. Try to establish a regular bowel habit by setting aside time each day, such as after a meal, to sit on the toilet.
-
Sitz Baths: Sitz baths, warm shallow baths for the hips and buttocks, are highly effective in relieving itching, irritation, and sphincter muscle spasms. Use a sitz bath after each bowel movement and 2-3 times daily for about 20 minutes. Gently pat the anal area dry afterward, avoiding harsh rubbing. A hair dryer on a cool setting can also be used to dry the area.
-
Topical Treatments: Over-the-counter hemorrhoid creams, ointments, and suppositories containing local anesthetics, corticosteroids, or protectants can provide temporary relief from pain, itching, and inflammation. Witch hazel wipes (like Tucks) can be soothing. Cold compresses or ice packs applied to the anal area for short periods can also help reduce swelling and pain.
-
Use Cushions: Sitting on a cushion instead of hard surfaces can reduce pressure on hemorrhoids and help prevent new ones from forming.
-
Treating Thrombosed External Hemorrhoids at Home: If the pain of a thrombosed external hemorrhoid is tolerable and has been present for more than 48 hours, home treatments may be sufficient to manage symptoms while waiting for it to resolve. However, if the pain is severe and recent, medical intervention might be considered.
Medical Procedures for Hemorrhoids: When Professional Help is Needed
When conservative treatments are not enough, or for more severe cases, several minimally invasive procedures and surgical options are available. These procedures are generally less painful and offer quicker recovery compared to traditional hemorrhoid surgery.
-
Rubber Band Ligation: This is the most common procedure for treating internal hemorrhoids in the United States. A small rubber band is placed around the base of the hemorrhoid, cutting off its blood supply. The hemorrhoid shrinks and eventually falls off within a few days, typically in about a week. Multiple sessions (2-4), spaced 6-8 weeks apart, may be needed to treat all hemorrhoids. Complications are rare but can include mild pain, bleeding, or infection.
Rubber band ligation of hemorrhoid
Alt text: Illustration depicting a medical professional using a ligator to place a rubber band at the base of an internal hemorrhoid during a rubber band ligation procedure.
-
Other Office Procedures: Other minimally invasive office procedures include laser or infrared coagulation, sclerotherapy (injection of a chemical solution to shrink the hemorrhoid), and cryosurgery (freezing the hemorrhoid). These methods work on similar principles to rubber band ligation but may vary in effectiveness and recurrence rates.
-
Hemorrhoidectomy: This is the traditional surgical removal of hemorrhoids and is typically reserved for large, protruding hemorrhoids, persistently symptomatic external hemorrhoids, or internal hemorrhoids that haven’t responded to other treatments. Hemorrhoidectomy is highly effective, curing about 95% of cases. While it has a reputation for being painful, modern pain management techniques have improved the recovery experience. It is usually performed under general anesthesia as an outpatient procedure, with a recovery time of 1-2 weeks before returning to work.
-
Stapled Hemorrhoidopexy: This procedure is an alternative to traditional hemorrhoidectomy, specifically for bleeding or prolapsed internal hemorrhoids. A stapling device is used to reposition the hemorrhoids back to their normal anatomical location within the anal canal. Like hemorrhoidectomy, it is performed under general anesthesia as day surgery.
Hemorrhoids are a common condition that can be effectively managed. While often uncomfortable and disruptive, understanding what hemorrhoids are, their causes, and the range of available treatments empowers individuals to seek appropriate care and find relief. From simple home remedies and lifestyle adjustments to minimally invasive procedures and surgery, there are solutions to address hemorrhoids and improve quality of life. If you suspect you have hemorrhoids or are experiencing rectal bleeding, it is always best to consult with a healthcare professional for proper diagnosis and personalized treatment recommendations.
