HSV1, or herpes simplex virus type 1, is a widespread infection. Want to understand more about it? WHAT.EDU.VN offers clear explanations and answers your questions. Let’s explore the transmission, management, and impact of this common virus and related information and insights. You can also ask specific questions on our site.
1. What is HSV1 and How Does It Differ From HSV2?
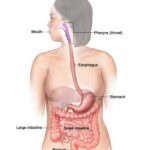
Herpes simplex virus type 1 (HSV-1) is a highly prevalent virus, with the World Health Organization (WHO) estimating that around 64% of the global population under 50 years old is infected. HSV-1 is primarily associated with oral herpes, commonly known as cold sores or fever blisters, which manifest as painful sores around the mouth and lips. However, it’s important to understand that HSV-1 can also cause genital herpes through oral-genital contact.
Herpes simplex virus type 2 (HSV-2), on the other hand, is mainly transmitted through sexual contact and is the primary cause of genital herpes. While both HSV-1 and HSV-2 can cause sores in the genital area, HSV-2 is more likely to result in recurrent outbreaks. Understanding the differences between these two viruses is crucial for managing and preventing their spread.
Here’s a quick comparison in a table:
| Feature | HSV-1 | HSV-2 |
|---|---|---|
| Primary Location | Oral (mouth, lips) | Genital area |
| Common Name | Oral herpes, cold sores, fever blisters | Genital herpes |
| Transmission | Oral contact, sometimes oral-genital contact | Sexual contact |
| Recurrence Rate | Lower for genital infections | Higher for genital infections |
| Global Prevalence | Higher | Lower |
Alt text: Close-up view of a cold sore, also known as a fever blister, on the corner of a human lip, indicating a common symptom of HSV-1 infection.
2. What are the Common Symptoms of HSV1?
Many individuals infected with HSV-1 may not experience any symptoms or may have very mild symptoms that go unnoticed. This is known as asymptomatic infection. However, when symptoms do appear, they can vary in severity and presentation.
Common symptoms of oral herpes (HSV-1) include:
- Cold Sores or Fever Blisters: These are small, painful blisters that typically occur on or around the lips. They may start as tingling or itching sensations before the blisters appear.
- Ulcers: Open sores that can develop when blisters rupture.
- Pain: Discomfort around the mouth and lips.
- Flu-like Symptoms: In some cases, particularly during the initial outbreak, individuals may experience fever, fatigue, and swollen lymph nodes.
Genital herpes caused by HSV-1 can present with similar symptoms to those caused by HSV-2, including:
- Blisters: Small, painful blisters on the genitals, buttocks, or inner thighs.
- Ulcers: Open sores that form when blisters break.
- Pain: Discomfort, itching, or burning sensations in the genital area.
- Flu-like Symptoms: Similar to oral herpes, the initial outbreak may be accompanied by fever, body aches, and swollen lymph nodes.
If you suspect you have HSV-1, it’s essential to consult with a healthcare professional for proper diagnosis and management.
3. How is HSV1 Transmitted?
Understanding how HSV-1 is transmitted is critical for preventing its spread. The virus is primarily transmitted through direct contact with the virus in sores, saliva, or skin surfaces.
Key routes of transmission include:
- Oral Contact: Kissing, sharing utensils, or sharing personal items like razors or towels can spread the virus.
- Oral-Genital Contact: Performing oral sex on someone with oral herpes can transmit HSV-1 to the genital area, causing genital herpes.
- Skin-to-Skin Contact: Direct contact with an active sore can spread the virus. However, it’s also possible to transmit HSV-1 even when no sores are present, through a process known as asymptomatic shedding.
- Mother to Child: In rare cases, a mother can transmit HSV-1 to her child during delivery, leading to neonatal herpes.
It’s important to note that once infected with HSV-1, the virus remains in the body for life. It lies dormant in nerve cells and can reactivate periodically, causing recurrent outbreaks.
Alt text: Illustrative diagram showing various routes of HSV-1 transmission including kissing, sharing utensils, and mother to child during delivery.
4. What are the Potential Triggers for HSV1 Outbreaks?
HSV-1 remains dormant in the body after the initial infection. Certain triggers can reactivate the virus, leading to recurrent outbreaks.
Common triggers include:
- Stress: Emotional or physical stress can weaken the immune system, making it easier for the virus to reactivate.
- Illness: Infections like colds or the flu can trigger outbreaks.
- Sun Exposure: Exposure to ultraviolet (UV) radiation can reactivate the virus, particularly around the mouth.
- Hormonal Changes: Menstruation or pregnancy can trigger outbreaks in some women.
- Trauma: Injury to the skin, such as cuts or abrasions, can reactivate the virus in that area.
- Weakened Immune System: Conditions or medications that suppress the immune system can increase the frequency and severity of outbreaks.
Identifying and managing these triggers can help reduce the frequency and severity of HSV-1 outbreaks.
5. How is HSV1 Diagnosed?
Diagnosing HSV-1 typically involves a physical examination and laboratory tests.
Common diagnostic methods include:
- Visual Examination: A healthcare provider can often diagnose herpes by visually examining the sores or blisters.
- Viral Culture: A sample taken from a sore can be tested to identify the presence of the virus.
- Polymerase Chain Reaction (PCR) Test: This test can detect the virus’s DNA in a sample taken from a sore or blood. PCR tests are highly sensitive and can identify the virus even when sores are not present.
- Antibody Tests: Blood tests can detect antibodies to HSV-1, indicating a past infection. However, these tests cannot determine the location of the infection (oral or genital).
If you suspect you have HSV-1, it’s important to seek medical attention for proper diagnosis and management.
6. What are the Available Treatment Options for HSV1?
While there is no cure for HSV-1, several treatment options can help manage symptoms and reduce the frequency and severity of outbreaks.
Common treatments include:
- Antiviral Medications: These medications, such as acyclovir, valacyclovir, and famciclovir, can help reduce the duration and severity of outbreaks. They work by interfering with the virus’s ability to replicate.
- Topical Creams: Topical antiviral creams, like acyclovir cream, can be applied directly to the sores to help them heal faster.
- Pain Relievers: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate pain and discomfort associated with outbreaks.
- Home Remedies: Some home remedies, such as applying a cold compress or using lip balms with sunscreen, can help soothe sores and promote healing.
Your healthcare provider can help you determine the most appropriate treatment plan based on your individual needs and the severity of your symptoms.
Alt text: Visual representation of various HSV-1 treatment options including antiviral medications, topical creams, and home remedies.
7. What are the Potential Complications of HSV1?
While HSV-1 is typically a mild infection, it can lead to complications in certain cases.
Potential complications include:
- Eye Infections (Herpetic Keratitis): HSV-1 can spread to the eyes, causing inflammation and potentially leading to vision loss.
- Encephalitis: In rare cases, HSV-1 can cause encephalitis, a serious inflammation of the brain.
- Neonatal Herpes: If a mother has genital herpes caused by HSV-1, she can transmit the virus to her baby during delivery, leading to neonatal herpes, a potentially life-threatening condition.
- Increased Risk of HIV Transmission: Individuals with genital herpes caused by either HSV-1 or HSV-2 are at an increased risk of acquiring and transmitting HIV.
- Psychological Impact: The stigma associated with herpes can lead to feelings of shame, anxiety, and depression.
It’s important to seek medical attention if you experience any unusual symptoms or complications related to HSV-1.
8. How Can HSV1 Transmission be Prevented?
Preventing the transmission of HSV-1 involves adopting certain precautions.
Key preventive measures include:
- Avoid Contact with Sores: Refrain from kissing or sharing personal items with someone who has an active outbreak.
- Practice Safe Sex: Use condoms during sexual activity to reduce the risk of genital herpes transmission.
- Inform Partners: If you have herpes, inform your sexual partners to allow them to make informed decisions about their health.
- Avoid Oral-Genital Contact: Avoid performing oral sex on someone with oral herpes.
- Wash Hands Frequently: Wash your hands thoroughly after touching a sore or applying medication.
- Avoid Sharing Personal Items: Do not share items that come into contact with saliva, such as toothbrushes, razors, or lip balm.
By taking these precautions, you can help reduce the risk of spreading HSV-1 to others.
9. What is the Impact of HSV1 on Pregnancy and Newborns?
HSV-1 can pose risks during pregnancy and to newborns. If a pregnant woman has genital herpes, there is a risk of transmitting the virus to her baby during delivery, leading to neonatal herpes.
Neonatal herpes can cause serious complications, including:
- Skin, Eye, and Mouth Infections: These infections can cause sores and blisters on the baby’s skin, eyes, and mouth.
- Brain Damage: In severe cases, neonatal herpes can cause encephalitis, leading to brain damage and developmental delays.
- Death: Neonatal herpes can be fatal, particularly if left untreated.
To prevent neonatal herpes, pregnant women with a history of genital herpes should inform their healthcare providers. Antiviral medications may be prescribed during the late stages of pregnancy to suppress the virus and reduce the risk of transmission to the baby. In some cases, a cesarean delivery may be recommended.
Alt text: A pregnant woman consulting with her healthcare provider about neonatal herpes prevention strategies during a prenatal checkup.
10. What are Some Common Misconceptions About HSV1?
There are several misconceptions about HSV-1 that can lead to confusion and stigma.
Common misconceptions include:
- Only People with Promiscuous Behavior Get Herpes: Anyone can contract herpes, regardless of their sexual history.
- Herpes is Just a Minor Inconvenience: While many people experience mild symptoms, herpes can cause significant pain, discomfort, and psychological distress.
- You Can’t Transmit Herpes When You Don’t Have Sores: Asymptomatic shedding can occur, meaning you can transmit the virus even when no sores are present.
- There is a Cure for Herpes: There is currently no cure for herpes, but treatments are available to manage symptoms and reduce the frequency of outbreaks.
- Herpes is a Rare Condition: HSV-1 and HSV-2 are very common infections worldwide.
Understanding the facts about HSV-1 can help reduce stigma and promote informed decision-making about sexual health.
11. What are the Psychological Effects of Living with HSV1?
Living with HSV-1 can have a significant psychological impact on individuals. The stigma associated with herpes can lead to feelings of shame, guilt, anxiety, and depression.
Common psychological effects include:
- Emotional Distress: Individuals may experience sadness, anger, or frustration related to their diagnosis.
- Low Self-Esteem: The presence of visible sores or the fear of transmitting the virus can lead to feelings of self-consciousness and low self-worth.
- Relationship Difficulties: Disclosure of herpes to a partner can be challenging and may lead to relationship issues.
- Social Isolation: Fear of judgment or rejection can cause individuals to withdraw from social activities.
- Anxiety and Depression: The chronic nature of herpes and the potential for recurrent outbreaks can contribute to anxiety and depression.
Seeking support from healthcare professionals, support groups, or therapists can help individuals cope with the psychological challenges of living with HSV-1.
12. What Lifestyle Changes Can Help Manage HSV1?
In addition to medical treatments, certain lifestyle changes can help manage HSV-1 and reduce the frequency and severity of outbreaks.
Helpful lifestyle changes include:
- Manage Stress: Practice stress-reducing techniques such as yoga, meditation, or deep breathing exercises.
- Maintain a Healthy Diet: Eat a balanced diet rich in fruits, vegetables, and whole grains to support your immune system.
- Get Enough Sleep: Aim for 7-8 hours of sleep per night to keep your immune system strong.
- Avoid Triggers: Identify and avoid triggers that can reactivate the virus, such as sun exposure, stress, or illness.
- Boost Your Immune System: Consider taking immune-boosting supplements, such as vitamin C, vitamin D, or zinc.
- Stay Hydrated: Drink plenty of water to keep your body functioning optimally.
These lifestyle changes can help you take control of your health and manage HSV-1 effectively.
13. Where Can I Find Reliable Information About HSV1?
Finding reliable information about HSV-1 is essential for making informed decisions about your health.
Trusted sources of information include:
- Healthcare Providers: Your doctor, nurse, or other healthcare professional can provide accurate and personalized information about HSV-1.
- World Health Organization (WHO): The WHO provides comprehensive information about herpes and other sexually transmitted infections.
- Centers for Disease Control and Prevention (CDC): The CDC offers detailed information about HSV-1, including prevention, diagnosis, and treatment.
- Reputable Medical Websites: Websites like Mayo Clinic, WebMD, and MedlinePlus offer reliable information about HSV-1.
- Support Groups: Connecting with others who have HSV-1 can provide valuable support and information.
Be cautious of unverified information found online or from unreliable sources. Always consult with a healthcare professional for personalized advice.
14. What Research is Being Conducted on HSV1?
Researchers are actively working to develop new strategies for preventing and treating HSV-1.
Current research areas include:
- Vaccine Development: Scientists are working to develop a vaccine that can prevent HSV-1 infection. Several vaccine candidates are currently in clinical trials.
- New Antiviral Medications: Researchers are developing new antiviral medications that are more effective and have fewer side effects than current treatments.
- Topical Microbicides: Topical microbicides are being developed to prevent the transmission of HSV-1 during sexual activity.
- Immunotherapy: Immunotherapy approaches are being explored to boost the immune system’s ability to control HSV-1 infection.
These research efforts offer hope for improved prevention and treatment options for HSV-1 in the future.
15. How Does HSV1 Affect Different Age Groups?
HSV-1 can affect individuals of all ages, but its impact can vary depending on the age group.
Here’s how HSV-1 affects different age groups:
- Children: Children often contract HSV-1 through contact with infected saliva, such as from kissing or sharing toys. Oral herpes is common in children and typically presents as cold sores around the mouth.
- Adolescents and Young Adults: Adolescents and young adults are at risk of contracting genital herpes caused by HSV-1 through oral-genital contact.
- Adults: Many adults have already been exposed to HSV-1 during childhood. However, they can still contract genital herpes caused by HSV-1 through sexual contact.
- Older Adults: Older adults may experience more frequent or severe outbreaks of HSV-1 due to a weakened immune system.
Understanding how HSV-1 affects different age groups can help tailor prevention and treatment strategies.
16. How Can Families Cope with HSV1 Diagnoses?
When a family member is diagnosed with HSV-1, it can impact the entire family.
Here are some tips for families coping with an HSV-1 diagnosis:
- Educate Yourselves: Learn about HSV-1, its transmission, and treatment options.
- Communicate Openly: Talk openly about the diagnosis and address any concerns or questions family members may have.
- Reduce Stigma: Challenge negative stereotypes about herpes and create a supportive environment.
- Practice Prevention: Take steps to prevent the spread of HSV-1 within the family, such as avoiding sharing personal items and practicing good hygiene.
- Seek Support: Consider joining a support group or seeking counseling to help cope with the emotional challenges of living with herpes.
- Be Empathetic: Show empathy and understanding towards the family member who has been diagnosed with HSV-1.
By working together, families can navigate the challenges of living with HSV-1 and provide support for one another.
17. What Role Does Diet Play in Managing HSV1?
While diet cannot cure HSV-1, it can play a role in managing the virus and reducing the frequency of outbreaks.
Dietary recommendations for managing HSV-1 include:
- Lysine-Rich Foods: Lysine is an amino acid that may help prevent HSV-1 outbreaks. Foods rich in lysine include legumes, fish, turkey, and chicken.
- Arginine-Poor Foods: Arginine is another amino acid that may promote HSV-1 replication. Foods high in arginine include nuts, seeds, chocolate, and coffee. Limiting these foods may help reduce outbreaks.
- Immune-Boosting Foods: Eat a diet rich in fruits, vegetables, and whole grains to support your immune system.
- Stay Hydrated: Drink plenty of water to keep your body functioning optimally.
- Avoid Processed Foods: Limit your intake of processed foods, which can weaken your immune system.
Consult with a healthcare professional or registered dietitian for personalized dietary recommendations.
18. Are There Natural Remedies for HSV1?
Some people explore natural remedies to manage HSV-1 symptoms and reduce outbreaks.
Natural remedies that may be helpful include:
- Lemon Balm: Lemon balm is an herb with antiviral properties that may help reduce the duration and severity of cold sores.
- Tea Tree Oil: Tea tree oil has antiseptic and antiviral properties that may help promote healing of cold sores.
- Aloe Vera: Aloe vera gel can help soothe and moisturize cold sores, reducing pain and inflammation.
- Propolis: Propolis is a resinous substance produced by bees that has antiviral and anti-inflammatory properties. It may help speed up the healing of cold sores.
- Echinacea: Echinacea is an herb that may boost the immune system and help prevent HSV-1 outbreaks.
It’s important to note that natural remedies may not be as effective as antiviral medications, and they may interact with other medications. Always consult with a healthcare professional before using natural remedies to manage HSV-1.
19. How Can I Support a Friend or Loved One with HSV1?
Supporting a friend or loved one with HSV-1 can make a significant difference in their well-being.
Here are some ways to provide support:
- Listen Without Judgment: Allow your friend or loved one to share their feelings and experiences without interruption or judgment.
- Offer Empathy and Understanding: Show empathy and understanding towards the challenges of living with herpes.
- Educate Yourself: Learn about HSV-1 to better understand what your friend or loved one is going through.
- Encourage Them to Seek Medical Care: Encourage them to see a healthcare professional for diagnosis and treatment.
- Be Respectful of Their Boundaries: Respect their boundaries regarding disclosure and sexual activity.
- Help Reduce Stigma: Challenge negative stereotypes about herpes and promote a supportive environment.
- Offer Practical Assistance: Offer help with errands, childcare, or other tasks to alleviate stress.
Your support can help your friend or loved one feel less alone and more empowered to manage their health.
20. What Questions Should I Ask My Doctor About HSV1?
If you suspect you have HSV-1 or have been diagnosed with the virus, it’s essential to ask your doctor the right questions.
Important questions to ask your doctor include:
- How Did I Contract HSV-1? Understanding how you contracted the virus can help you prevent future transmission.
- What are My Treatment Options? Discuss the available treatment options and their potential benefits and risks.
- How Can I Manage Outbreaks? Learn how to manage outbreaks and reduce their frequency and severity.
- How Can I Prevent Transmission to Others? Get advice on how to prevent transmitting the virus to sexual partners or family members.
- Are There Any Potential Complications? Discuss any potential complications of HSV-1 and how to monitor for them.
- What Lifestyle Changes Can I Make? Get recommendations for lifestyle changes that can help manage the virus.
- Where Can I Find Reliable Information and Support? Ask for recommendations for reliable sources of information and support groups.
- How Often Should I Come in for Follow-Up Appointments? Determine the appropriate frequency for follow-up appointments.
Asking these questions will help you gain a better understanding of HSV-1 and how to manage it effectively.
21. Understanding Asymptomatic Shedding of HSV1
Asymptomatic shedding refers to the release of the HSV-1 virus from the body even when there are no visible sores or symptoms present. This is a critical aspect of HSV-1 transmission because individuals can unknowingly transmit the virus to others. The frequency and duration of asymptomatic shedding vary among individuals. Factors like stress, immune system health, and overall health can influence the likelihood of shedding.
Preventive measures are crucial even in the absence of symptoms. Consistent and correct use of condoms can reduce the risk of genital herpes transmission. Avoiding direct contact, such as kissing or sharing personal items, can also help prevent the spread of oral herpes. Regular communication with sexual partners about herpes status is vital for informed decision-making and reducing transmission risks.
22. HSV1 and its Impact on Mental and Emotional Well-being
Living with HSV1 can significantly impact mental and emotional well-being. The stigma associated with herpes can lead to feelings of shame, guilt, anxiety, and depression. The visible symptoms, such as cold sores, can also cause self-consciousness and affect self-esteem. Furthermore, the chronic nature of the infection and the possibility of recurrent outbreaks can contribute to stress and uncertainty.
Addressing these psychological challenges is essential for overall well-being. Seeking support from healthcare professionals, such as therapists or counselors, can provide valuable coping strategies and emotional support. Joining support groups or online communities can connect individuals with others who understand their experiences, reducing feelings of isolation. Practicing self-care activities, such as exercise, meditation, and hobbies, can help manage stress and improve mood.
23. The Role of the Immune System in HSV1 Management
The immune system plays a crucial role in controlling HSV1 infection. A strong and healthy immune system can help suppress the virus, reduce the frequency and severity of outbreaks, and minimize asymptomatic shedding. Several factors can influence immune system function, including diet, lifestyle, and underlying health conditions.
Adopting lifestyle habits that support immune function is essential for managing HSV1. Eating a balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients that support immune cell function. Regular exercise helps boost immune cell activity and reduce inflammation. Getting enough sleep is vital for immune system regulation and repair. Managing stress through relaxation techniques, such as yoga or meditation, can prevent immune system suppression.
Alt text: Diagram illustrating the role of the human immune system in managing the herpes simplex virus type 1 infection, emphasizing the importance of a healthy diet and lifestyle.
24. Navigating Relationships and Disclosure with HSV1
Disclosing a herpes diagnosis to a sexual partner can be a challenging but essential step in building trust and ensuring informed consent. It’s important to choose the right time and place for the conversation, and to be honest and open about your diagnosis. Providing accurate information about herpes transmission, prevention, and management can help alleviate concerns and reduce stigma.
When navigating relationships with HSV1, communication is key. Discussing sexual health history, practicing safe sex, and respecting each other’s boundaries are vital for maintaining a healthy and fulfilling relationship. Remember that having herpes does not define you, and it should not prevent you from having meaningful connections with others.
25. HSV1 Prevention Strategies for Expecting Mothers
Preventing HSV1 transmission from mother to child during pregnancy and childbirth is crucial for protecting newborns from neonatal herpes. Pregnant women with a history of herpes should inform their healthcare providers, as antiviral medications may be prescribed during the late stages of pregnancy to suppress the virus and reduce the risk of transmission. In some cases, a cesarean delivery may be recommended.
Newborns who contract herpes can experience serious complications, including skin, eye, and mouth infections, brain damage, and even death. Early diagnosis and treatment are essential for improving outcomes. Healthcare providers closely monitor newborns for signs of herpes infection and administer antiviral medications as needed.
Do you have more questions about HSV1 or any other health concerns? At WHAT.EDU.VN, we provide a platform where you can ask any question and receive answers quickly and for free. Our goal is to provide you with easy-to-understand and helpful information.
Are you struggling to find answers to your questions? Do you need reliable information without the hassle? Visit WHAT.EDU.VN today and ask your question. Our community of experts is ready to provide you with the answers you need, absolutely free.
Address: 888 Question City Plaza, Seattle, WA 98101, United States
WhatsApp: +1 (206) 555-7890
Website: what.edu.vn