Refeeding syndrome is a dangerous condition involving fluid and electrolyte shifts in malnourished patients undergoing artificial refeeding. At WHAT.EDU.VN, we aim to provide comprehensive insights into this syndrome, its prevention, and treatment. Discover how to identify risk factors, manage electrolyte imbalances, and ensure patient safety with our easy to understand guidance, ultimately preventing metabolic complications and promoting nutritional recovery.
1. Defining Refeeding Syndrome: What Exactly Is It?
Refeeding syndrome is a potentially fatal metabolic disturbance that can occur when nutrition is reintroduced too quickly after a period of starvation or significant malnutrition. It’s characterized by dramatic shifts in fluids and electrolytes that can overwhelm the body and lead to severe complications. Refeeding syndrome represents a significant challenge in nutritional management, particularly for individuals with compromised nutritional status.
1.1. The Core Components of Refeeding Syndrome
The hallmark of refeeding syndrome is hypophosphatemia (low phosphate levels in the blood). However, this is just one piece of the puzzle. Other key features include:
- Electrolyte Imbalances: Shifts in potassium (hypokalemia), magnesium (hypomagnesemia), and sodium levels.
- Fluid Overload: Rapid changes in fluid balance, potentially leading to edema and heart failure.
- Metabolic Changes: Alterations in glucose, protein, and fat metabolism.
- Vitamin Deficiencies: Particularly thiamine deficiency, which can cause neurological complications.
1.2. Why Is Refeeding Syndrome Dangerous?
The rapid introduction of nutrients after starvation triggers a cascade of hormonal and metabolic changes. Insulin secretion increases, driving electrolytes and glucose into cells. This sudden shift can lead to:
- Cardiac Arrhythmias: Electrolyte imbalances can disrupt heart function.
- Respiratory Failure: Fluid overload and electrolyte imbalances can compromise lung function.
- Neurological Problems: Thiamine deficiency can cause Wernicke’s encephalopathy.
- Death: In severe cases, refeeding syndrome can be fatal.
1.3. Key Takeaway
Refeeding syndrome is a complex metabolic condition that demands careful management and awareness. Early identification and preventative strategies are crucial for minimizing risks and ensuring successful nutritional rehabilitation. If you have more questions, remember you can always ask them for free on WHAT.EDU.VN.
2. Understanding the Prevalence: How Common Is Refeeding Syndrome?
Determining the exact prevalence of refeeding syndrome is challenging due to variations in diagnostic criteria and inconsistent recognition of the condition. However, studies provide some insights into its occurrence, particularly in hospitalized patients.
2.1. Incidence of Hypophosphatemia
Hypophosphatemia, a key marker of refeeding syndrome, has been studied in various populations. One study involving 10,197 hospitalized patients found the incidence of severe hypophosphatemia to be 0.43%, with malnutrition identified as a strong risk factor.
2.2. Impact of Phosphate-Free Solutions
The use of total parenteral nutrition (TPN) solutions lacking phosphate has been linked to a high incidence of hypophosphatemia. Studies have reported a 100% incidence of hypophosphatemia in patients receiving such solutions. However, when phosphate-containing solutions are used, the incidence can decrease to around 18%.
2.3. Refeeding Syndrome in Intensive Care Units
Prospective and retrospective cohort studies in intensive care units (ICUs) have documented the occurrence of refeeding syndrome. A prospective study of a diverse group of ICU patients found that 34% experienced hypophosphatemia shortly after the initiation of feeding (mean 1.9 days).
2.4. The Under-Recognition Challenge
Despite the documented cases and potential severity, refeeding syndrome is often under-recognized and may be inappropriately treated, particularly on general hospital wards. This highlights the need for increased awareness and education among healthcare professionals.
2.5. What These Statistics Mean
These figures indicate that while severe refeeding syndrome may not be common in the general population, it poses a significant risk in specific patient groups, especially those with malnutrition and those receiving artificial nutrition. If you’re curious about the specific diagnostic criteria used in these studies, remember that you can always ask a medical professional on WHAT.EDU.VN.
3. The Development of Refeeding Syndrome: A Step-by-Step Look
To understand how to prevent and treat refeeding syndrome, it’s crucial to grasp the underlying physiological processes that lead to its development. It’s a cascade of events triggered by the body’s response to renewed nutrition after a period of starvation.
3.1. The Fasting State
During prolonged fasting, the body undergoes significant metabolic and hormonal adaptations to conserve energy and preserve vital functions. Here’s what happens:
- Fuel Source Shift: The body switches from using carbohydrates to fat and protein as its primary energy source.
- Basal Metabolic Rate Reduction: The basal metabolic rate can decrease by as much as 20-25% to conserve energy.
- Ketone Body Production: The liver produces ketone bodies from fat, which become an important energy source for the brain.
- Gluconeogenesis Reduction: The liver decreases its rate of gluconeogenesis (glucose production from non-carbohydrate sources) to preserve muscle protein.
- Intracellular Mineral Depletion: Intracellular minerals, such as phosphate, potassium, and magnesium, become severely depleted, though serum concentrations may remain normal.
- Renal Excretion Reduction: The kidneys reduce the excretion of electrolytes to conserve them.
3.2. The Refeeding State
When refeeding begins, the sudden influx of nutrients triggers a reversal of the metabolic adaptations that occurred during fasting:
- Glycemia Increase: Increased glucose levels lead to increased insulin secretion and decreased glucagon secretion.
- Glycogen, Fat, and Protein Synthesis: Insulin stimulates the synthesis of glycogen (stored glucose), fat, and protein.
- Mineral Demand: These synthetic processes require minerals such as phosphate and magnesium, as well as cofactors like thiamine.
- Electrolyte Shift: Insulin stimulates the absorption of potassium, magnesium, and phosphate into cells, leading to a decrease in serum levels.
- Water Retention: Water follows electrolytes into cells by osmosis, contributing to fluid shifts.
- Basal Metabolic Rate Increase: The basal metabolic rate increases as the body resumes its normal metabolic processes.
3.3. The Consequences
The rapid shifts in electrolytes, fluids, and metabolic rate can overwhelm the body, leading to the clinical features of refeeding syndrome. If you’re wondering what the timeline is for these changes, remember that you can always ask a medical professional on WHAT.EDU.VN.
4. Electrolytes and Minerals: The Key Players in Refeeding Syndrome
Several electrolytes and minerals play crucial roles in the pathogenesis of refeeding syndrome. Understanding their functions and how they are affected by refeeding is essential for effective prevention and treatment.
4.1. Phosphorus
- Function: Phosphorus is a predominantly intracellular mineral essential for all intracellular processes, cell membrane integrity, enzyme activation, energy storage (ATP), oxygen delivery to tissues, and renal acid-base buffering.
- In Refeeding Syndrome: Chronic whole-body depletion of phosphorus occurs during starvation. The insulin surge during refeeding causes a greatly increased uptake and use of phosphate in the cells, leading to a deficit in both intracellular and extracellular phosphorus.
- Consequences: Even small decreases in serum phosphorus can lead to widespread dysfunction of cellular processes, affecting almost every physiological system.
4.2. Potassium
- Function: Potassium is the major intracellular cation, crucial for maintaining electrochemical membrane potential, nerve impulse transmission, and muscle contraction.
- In Refeeding Syndrome: Potassium is depleted in undernutrition, but serum concentration may remain normal. With refeeding, potassium is taken up into cells, leading to severe hypokalemia.
- Consequences: Hypokalemia causes derangements in the electrochemical membrane potential, resulting in arrhythmias and cardiac arrest.
4.3. Magnesium
- Function: Magnesium is an important cofactor in most enzyme systems, including oxidative phosphorylation and ATP production. It is also necessary for the structural integrity of DNA, RNA, and ribosomes, and affects membrane potential.
- In Refeeding Syndrome: Magnesium is depleted in undernutrition. Refeeding can exacerbate this depletion, leading to hypomagnesemia.
- Consequences: Magnesium deficiency can lead to cardiac dysfunction and neuromuscular complications.
4.4. Glucose
- Function: Glucose is the primary source of energy for the body.
- In Refeeding Syndrome: Excessive glucose administration after starvation can lead to hyperglycemia.
- Consequences: Hyperglycemia can cause osmotic diuresis, dehydration, metabolic acidosis, ketoacidosis, lipogenesis, fatty liver, increased carbon dioxide production, hypercapnoea, and respiratory failure.
4.5. Thiamine
- Function: Thiamine is an essential coenzyme in carbohydrate metabolism.
- In Refeeding Syndrome: Thiamine deficiency is a significant concern in refeeding.
- Consequences: Thiamine deficiency can result in Wernicke’s encephalopathy (ocular abnormalities, ataxia, confusional state, hypothermia, coma) or Korsakoff’s syndrome (retrograde and anterograde amnesia, confabulation).
4.6. Sodium and Fluids
- Function: Sodium and fluids are crucial for maintaining fluid balance and blood pressure.
- In Refeeding Syndrome: The introduction of carbohydrate leads to a rapid decrease in renal excretion of sodium and water.
- Consequences: If fluid repletion is instituted to maintain normal urine output, patients may rapidly develop fluid overload, leading to congestive heart failure, pulmonary edema, and cardiac arrhythmia.
4.7. Key Takeaway
Electrolyte and mineral imbalances are at the heart of refeeding syndrome. Monitoring and managing these imbalances is crucial for preventing serious complications. If you’re looking for specific monitoring guidelines, remember that you can always ask a medical professional on WHAT.EDU.VN.
5. Preventing Refeeding Syndrome: A Proactive Approach
Preventing refeeding syndrome is far better than treating it. Identifying high-risk patients and implementing appropriate refeeding strategies are crucial.
5.1. Identifying High-Risk Patients
Any patient with negligible food intake for more than five days is at risk of developing refeeding problems. High-risk patients include those who have been chronically undernourished, especially those with diminished physiological reserve.
Conditions that Increase Risk:
- Reduced intake (e.g., dysphagia, anorexia nervosa, depression, alcoholism)
- Reduced absorption of nutrition (e.g., inflammatory bowel disease, coeliac disease)
- Increased metabolic demands (e.g., cancer, surgery)
- Chronic alcoholism
- Oncology patients
- Postoperative patients
- Elderly patients (comorbidities, decreased physiological reserve)
- Patients with uncontrolled diabetes mellitus (electrolyte depletion, diuresis)
- Patients with chronic malnutrition (marasmus, prolonged fasting, morbid obesity with profound weight loss, high stress patient unfed for >7 days, malabsorptive syndrome)
- Long-term users of antacids (magnesium and aluminum salts bind phosphate)
- Long-term users of diuretics (loss of electrolytes)
5.2. NICE Guidelines for Identifying High-Risk Patients
The National Institute for Health and Clinical Excellence (NICE) provides specific criteria for identifying patients at high risk of refeeding problems:
One or More of the Following:
- Body mass index (BMI) <16 kg/m2
- Unintentional weight loss >15% in the past three to six months
- Little or no nutritional intake for >10 days
- Low levels of potassium, phosphate, or magnesium before feeding
Or Two or More of the Following:
- Body mass index <18.5 kg/m2
- Unintentional weight loss >10% in the past three to six months
- Little or no nutritional intake for >5 days
- History of alcohol misuse or drugs, including insulin, chemotherapy, antacids, or diuretics
5.3. Nutritional Assessment Before Refeeding
A thorough nutritional assessment should be conducted before refeeding is started. This assessment should include:
- Recent weight change over time
- Nutrition history
- Alcohol intake
- Social and psychological problems
- Plasma electrolytes (especially phosphate, sodium, potassium, and magnesium)
- Glucose levels
5.4. Gradual Refeeding
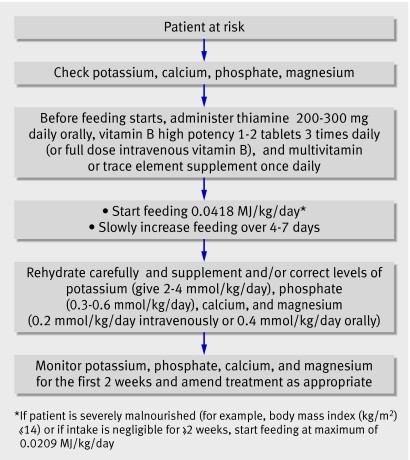
Refeeding should be started slowly to avoid overwhelming the body with nutrients. The NICE guidelines recommend:
- Patients who have eaten little or nothing for more than 5 days: Start at no more than 50% of energy requirements.
- High-risk patients: Start nutritional repletion of energy slowly (maximum 0.042 MJ/kg/24 hours) and tailor to each patient, increasing to meet full needs over four to seven days.
- Very malnourished patients (BMI ≤14 or negligible intake for two weeks or more): Start at a maximum of 0.021 MJ/kg/24 hours, with cardiac monitoring due to the risk of cardiac arrhythmias.
5.5. Electrolyte and Fluid Management
Electrolyte and fluid imbalances should be corrected during feeding, not necessarily before. Vitamin supplementation should be started immediately, before and for the first 10 days of refeeding. Circulatory volume should also be restored.
5.6. Supplementation
Oral, enteral, or intravenous supplements of potassium, phosphate, calcium, and magnesium should be given unless blood levels are high before refeeding.
5.7. Monitoring
Electrolyte levels should be measured once daily for one week and at least three times in the following week. Urinary electrolytes could also be checked to help assess body losses and guide replacement.
5.8. Key Takeaway
Preventing refeeding syndrome requires a multi-faceted approach that includes identifying high-risk patients, conducting thorough nutritional assessments, implementing gradual refeeding strategies, and closely monitoring electrolyte and fluid balance. If you’re looking for a checklist to ensure you’re covering all the bases, remember that you can always ask a medical professional on WHAT.EDU.VN.
 patient at high risk of refeeding syndrome
patient at high risk of refeeding syndrome
6. Detecting and Treating Refeeding Syndrome: A Step-by-Step Guide
Despite the best preventative efforts, refeeding syndrome can still occur. Early detection and prompt treatment are crucial for minimizing complications and ensuring patient safety.
6.1. Detection
Refeeding syndrome is detected by considering the possibility of its existence in at-risk patients and by using simple biochemical investigations.
Key Investigations:
- Plasma electrolytes (especially phosphate, sodium, potassium, and magnesium)
- Glucose levels
- Renal function tests
- Cardiac monitoring (in severe cases)
6.2. Treatment
If refeeding syndrome is detected, the rate of feeding should be slowed down, and essential electrolytes should be replenished. The hospital specialist dietetics team should be involved.
Key Treatment Strategies:
- Slow Down Refeeding: Reduce the rate of nutrient administration to allow the body to adjust.
- Electrolyte Repletion: Replace deficient electrolytes, such as phosphate, potassium, and magnesium, through intravenous or oral supplementation.
- Fluid Management: Carefully control fluid administration to avoid fluid overload.
- Vitamin Supplementation: Continue thiamine and other vitamin supplementation.
- Cardiac Monitoring: Monitor cardiac function closely, especially in patients with severe electrolyte imbalances.
6.3. Electrolyte Repletion Strategies
The best method for electrolyte repletion has not yet been definitively determined. Intravenous supplementation is often preferred in hospitalized patients, but it is not without risks.
Phosphate Supplementation:
- Mild Hypophosphatemia (0.6-0.85 mmol/l): 0.3-0.6 mmol/kg/day orally
- Moderate Hypophosphatemia (0.3-0.6 mmol/l): 9 mmol infused into peripheral vein over 12 hours
- Severe Hypophosphatemia (<0.3 mmol/l): 18 mmol infused into peripheral vein over 12 hours
Magnesium Supplementation:
- Mild to Moderate Hypomagnesemia (0.5-0.7 mmol/l): Initially 0.5 mmol/kg/day over 24 hours intravenously, then 0.25 mmol/kg/day for 5 days intravenously
- Severe Hypomagnesemia (<0.5 mmol/l): 24 mmol over 6 hours intravenously, then as for mild to moderate hypomagnesemia
Important Considerations:
- Careful monitoring of blood levels is required during electrolyte repletion.
- Caution is needed in patients with existing renal impairment, hypocalcemia (which may worsen), or hypercalcemia (which may result in metastatic calcification).
6.4. Fluid Management
Fluid repletion should be carefully controlled to avoid fluid overload. Sodium administration should be limited to the replacement of losses. In patients at high risk of cardiac decompensation, central venous pressure and cardiac rhythm monitoring should be considered.
6.5. Key Takeaway
Detecting and treating refeeding syndrome requires a vigilant approach that includes recognizing at-risk patients, monitoring biochemical parameters, and implementing prompt and appropriate interventions. If you’re looking for a detailed protocol for managing refeeding syndrome, remember that you can always ask a medical professional on WHAT.EDU.VN.
7. Refeeding Syndrome: Frequently Asked Questions (FAQ)
Here are some frequently asked questions about refeeding syndrome, designed to provide quick and clear answers:
| Question | Answer |
|---|---|
| What is the main cause of refeeding syndrome? | The main cause is the rapid introduction of nutrients after a period of starvation or malnutrition, leading to sudden shifts in electrolytes and fluids. |
| What is the hallmark biochemical feature of refeeding syndrome? | Hypophosphatemia (low phosphate levels in the blood) is the hallmark biochemical feature. |
| Who is at high risk of developing refeeding syndrome? | Patients with anorexia nervosa, chronic alcoholism, oncology patients, postoperative patients, elderly patients, patients with uncontrolled diabetes, and those with chronic malnutrition are at high risk. |
| How can refeeding syndrome be prevented? | Prevention involves identifying high-risk patients, conducting thorough nutritional assessments, starting refeeding slowly, monitoring electrolytes and fluids, and providing appropriate vitamin and mineral supplementation. |
| What are the NICE guidelines for identifying high-risk patients? | The NICE guidelines include criteria such as low BMI, unintentional weight loss, little or no nutritional intake for a certain period, and a history of alcohol or drug misuse. |
| What is the recommended rate of refeeding for high-risk patients? | For high-risk patients, nutritional repletion should be started slowly (maximum 0.042 MJ/kg/24 hours) and tailored to each patient, increasing to meet full needs over four to seven days. For very malnourished patients, start at a maximum of 0.021 MJ/kg/24 hours. |
| What electrolytes should be monitored during refeeding? | Electrolytes that should be monitored include phosphate, sodium, potassium, and magnesium. |
| What vitamins are particularly important in preventing refeeding syndrome? | Thiamine is particularly important, as thiamine deficiency can lead to Wernicke’s encephalopathy. |
| How is refeeding syndrome treated? | Treatment involves slowing down the rate of feeding, replenishing deficient electrolytes, carefully managing fluids, and providing vitamin supplementation. |
| What are the potential complications of refeeding syndrome? | Potential complications include cardiac arrhythmias, respiratory failure, neurological problems, and death. |
| Where can I ask more questions about refeeding syndrome and get personalized answers? | You can visit WHAT.EDU.VN to ask questions and receive free answers from our community of experts and other knowledgeable users. |
This table summarizes key information about refeeding syndrome, offering a quick reference for understanding, prevention, and treatment.
8. Conclusion: A Call to Action
Refeeding syndrome is a serious but preventable and treatable condition. By increasing awareness, implementing preventative strategies, and providing prompt treatment, healthcare professionals can significantly reduce the incidence and associated complications of this syndrome.
Remember, you’re not alone in your quest for knowledge and understanding. Whether you’re a healthcare professional seeking to refine your skills or an individual with personal questions, WHAT.EDU.VN is here to provide the answers you need. Visit us at WHAT.EDU.VN, where asking questions is always free.
Need Answers? Ask Us Anything!
Do you have specific questions about refeeding syndrome or any other health-related topic? Don’t hesitate to reach out. Our platform is designed to connect you with experts and provide you with the information you need. Visit WHAT.EDU.VN today and start asking!
Contact Information:
- Address: 888 Question City Plaza, Seattle, WA 98101, United States
- WhatsApp: +1 (206) 555-7890
- Website: WHAT.EDU.VN
At what.edu.vn, we believe that everyone deserves access to reliable, accurate information. Let us help you on your journey to better health and understanding. Start asking questions today!