Several genetic alterations have been identified that can elevate the risk of developing Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) in response to certain triggers, most notably medications. These genetic changes primarily affect genes critical for the proper functioning of the immune system.
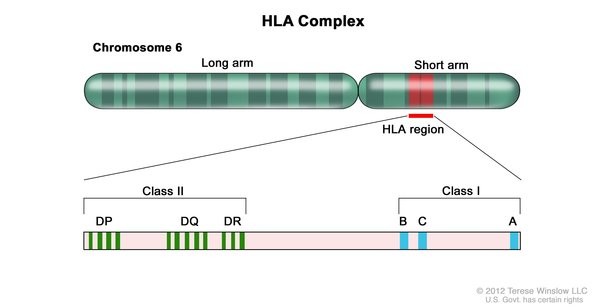
The most significant genetic links to SJS/TEN are found in the HLA-B gene. This gene belongs to the human leukocyte antigen (HLA) complex, a group of genes crucial for the immune system’s ability to distinguish between the body’s own proteins and foreign proteins from invaders like viruses and bacteria. The HLA-B gene has many variations, enabling the immune system to respond to a wide array of foreign proteins. However, specific variations in this gene are observed much more frequently in individuals with SJS/TEN compared to those without the condition.
Research indicates that specific HLA-B gene variations associated with SJS/TEN can cause the immune system to react abnormally to certain medications. In a poorly understood process, the drug triggers cytotoxic T cells and natural killer (NK) cells (types of immune cells) to release granulysin, a substance that destroys cells in the skin and mucous membranes. This cellular destruction leads to the characteristic blistering and peeling observed in SJS/TEN.
While variations in other HLA and non-HLA genes have been explored as potential risk factors for SJS/TEN, the majority of individuals with these genetic variations never develop the disease, even when exposed to triggering drugs. This suggests that additional genetic and non-genetic factors, many of which remain unknown, likely influence whether someone develops SJS/TEN. The role of genetic predisposition, particularly concerning HLA-B gene variants, is a key area of ongoing research to predict susceptibility and improve patient outcomes.
Medications commonly linked to SJS/TEN include certain anti-seizure drugs (such as carbamazepine, lamotrigine, and phenytoin), allopurinol (used for kidney stones and gout), sulfonamide antibiotics, nevirapine (used to treat HIV), and oxicams (a type of non-steroidal anti-inflammatory drug or NSAID). Other triggers may also exist. For instance, SJS/TEN has been observed in individuals with atypical pneumonia caused by Mycoplasma pneumoniae and in those with viral infections like cytomegalovirus. Researchers hypothesize that a combination of infections and drugs may contribute to the disease in some cases. Often, a definitive trigger for an individual’s SJS/TEN is never identified. Understanding these triggers and the genetic factors involved is crucial for better diagnosis, prevention, and treatment strategies.