Thrombosis occurs when a blood clot forms abnormally inside a blood vessel. Medical professionals often refer to this clot as a thrombus. This formation obstructs the normal flow of blood within the circulatory system. Without proper blood circulation, tissues and vital organs, such as the heart, are deprived of essential nutrients and oxygen.
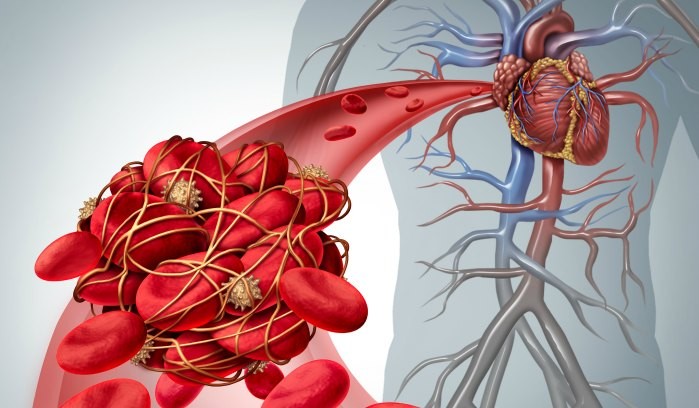 Illustration depicting a blood clot obstructing a vein, highlighting the condition of thrombosis and its impact on blood flow.
Illustration depicting a blood clot obstructing a vein, highlighting the condition of thrombosis and its impact on blood flow.
Blood clots that develop and remain stationary in a blood vessel are known as thrombi. Conversely, when a blood clot breaks loose and travels through the bloodstream, it is termed an embolus. Thrombosis can manifest in both arteries and veins. The approach to treatment is determined by the specific type of thrombosis, its severity, and the clot’s location within the body.
What Causes Thrombosis?
Blood clotting, scientifically known as coagulation, is a crucial bodily defense mechanism against bleeding. When a blood vessel sustains an injury, such as a cut, the body activates the coagulation system. This system works to create a “plug” at the injury site, effectively halting further blood loss. Typically, once the injury heals, the body naturally dissolves the clot. However, in some instances, this breakdown process fails to occur.
Blood clots can also arise due to factors unrelated to vessel injury. Certain medical conditions, medications, or medical treatments can lead to an increased thickness of the blood, thereby elevating the likelihood of clot formation. In situations where blood flow is sluggish due to prolonged inactivity, blood can accumulate or stagnate in place. Blood that remains stationary for extended periods is more prone to clotting.
Types of Thrombosis
There are primarily two categories of thrombosis:
- Arterial Thrombosis: This type occurs when a blood clot develops in an artery. Arteries are responsible for transporting oxygen-rich blood away from the heart to the body’s tissues and organs. Arterial thrombosis can severely restrict or completely block blood flow, leading to serious conditions such as heart attack or stroke if it occurs in the arteries supplying the heart or brain, respectively.
- Venous Thrombosis: This type involves the formation of a blood clot in a vein. Veins carry blood back to the heart from the rest of the body. The most common form of venous thrombosis is deep vein thrombosis (DVT), which typically occurs in the deep veins of the legs. Another significant concern is pulmonary embolism (PE), which happens when a DVT clot breaks free and travels to the lungs, obstructing blood flow there.
Thrombosis Risk Factors
Certain factors can elevate an individual’s susceptibility to developing thrombosis. These risk factors include:
- Surgery: Post-operative periods, especially major surgeries, can increase clot risk due to immobility and tissue injury.
- Obesity: Excess weight is linked to increased clotting factors in the blood.
- Smoking: Smoking damages blood vessels and increases blood thickness and stickiness.
- Diabetes: High blood sugar levels can damage blood vessels, making clots more likely.
- Infections: Severe infections can activate the clotting system excessively.
- Pregnancy: Hormonal changes and pressure on veins during pregnancy increase clot risk.
- Major Trauma: Severe injuries can trigger the clotting process.
- Atrial Fibrillation: This irregular heart rhythm can lead to stagnant blood in the heart, promoting clot formation.
- Family History of Clots: Genetic predisposition can increase the likelihood of thrombosis.
- Limited Physical Activity: Prolonged immobility, such as during long flights or bed rest, slows blood flow.
- Cancer and Chemotherapy: Certain cancers and their treatments can increase clotting risk.
- Inflammatory or Autoimmune Diseases: Conditions like lupus or rheumatoid arthritis can elevate clot risk.
- Genetic or Acquired Clotting Disorders: Inherited or developed conditions that make blood clot too easily.
- Atherosclerosis: Plaque buildup in arteries can narrow vessels and promote clot formation.
- Estrogen-Containing Contraceptives and Hormone Replacement Therapy: These can increase clotting factors.
Can Blood Clots Be Dissolved or Removed?
While the body can naturally dissolve blood clots over time, this process can take weeks or even years. Some clots require medical intervention to resolve. Treatment strategies depend on the clot type, location, and severity. Common treatments include:
- Thrombolytics: These medications, administered intravenously, are designed to dissolve clots rapidly and restore blood flow.
- Catheter-Directed Thrombolysis: This targeted approach involves guiding a catheter to the clot’s location and delivering thrombolytic drugs directly to it.
- Surgery (Thrombectomy): In critical situations like severe strokes, heart attacks, or pulmonary embolisms, surgical removal of the clot may be necessary.
- Anticoagulants (Blood Thinners): These medications don’t dissolve existing clots but prevent new ones from forming and can help the body’s natural processes dissolve the current clot, while also reducing the risk of clot growth.
What are the Risks of Blood Clot Recurrence?
The likelihood of experiencing another blood clot varies depending on the initial cause. Clots triggered by temporary factors like surgery or trauma have a lower recurrence risk. However, individuals who develop clots without an obvious cause (unprovoked clots) face a higher chance of recurrence, even after treatment. Studies indicate a recurrence rate of approximately 20% within the first four years and around 30% after ten years for those who discontinue anticoagulant therapy after an unprovoked event.
What are the Risks of Taking Anticoagulants (Blood Thinners)?
Anticoagulants, while crucial for preventing and treating thrombosis, inherently increase the risk of bleeding. Signs of excessive bleeding may include prolonged nosebleeds, unexplained bruising, bleeding gums, vomiting blood, coughing up blood, or, in women, unusually heavy menstrual bleeding.
Individuals on blood thinners should seek immediate medical attention for:
- Head trauma
- Major accidents, such as car crashes
- Unstoppable or prolonged bleeding
Despite the bleeding risk, anticoagulants are vital for managing thrombosis. Patients should never discontinue these medications without consulting their healthcare provider. Any concerns about blood thinners, including affordability issues, should be discussed with a doctor or pharmacist.
Recently Diagnosed?
For those seeking further information or support, numerous resources are available. Patient support groups and educational materials can provide valuable assistance in understanding and managing thrombosis.
See Resources
References
Ashorobi D, Ameer MA, Fernandez R. Thrombosis. In: StatPearls. StatPearls Publishing; 2024. Accessed on June 6, 2024.
Baig MU, BJ. Thrombolytic therapy. In: StatPearls. StatPearls Publishing; 2024. Accessed on June 5, 2024.
Blood Clots. American Society of Hematology. Accessed on June 5, 2024. https://www.hematology.org/education/patients/blood-clots
Blood Clots. Medlineplus.gov. Accessed June 5, 2024. https://medlineplus.gov/bloodclots.html
Centers for Disease Control and Prevention. Data and Statistics on Venous Thromboembolism. Venous Thromboembolism (Blood Clots). Published on May 15, 2024. https://www.cdc.gov/blood-clots/data-research/facts-stats/index.html
Mathews S, De Jesus O. Thrombectomy. In: StatPearls. StatPearls Publishing; 2024. Accessed on June 5, 2024.
Mount HR, Rich M, Putnam MS. Recurrent venous thromboembolism. American Family Physician. 2022;105(4):377-385.
The basics of blood clots: What you need to know. NIH MedlinePlus Magazine. Accessed on June 6, 2024. https://magazine.medlineplus.gov/article/the-basics-of-blood-clots-what-you-need-to-know