A polyp is an abnormal tissue growth in the body, and WHAT.EDU.VN is here to provide you with comprehensive information about it. This growth can occur in various organs, including the colon, nose, throat, uterus, and more, sometimes requiring medical attention. Explore this guide to understand polyp types, symptoms, and management. Learn about polyp prevention, precancerous polyps, and benign polyps.
1. What Exactly Is a Polyp Medically Speaking?
A polyp is essentially an abnormal growth of tissue projecting from a mucous membrane. These growths can be found in various parts of the body, including the colon, nasal passages, stomach, uterus, and even the ears. While many polyps are benign, meaning they are not cancerous, some can be precancerous or even cancerous.
Understanding the nature of a polyp is crucial for determining the appropriate course of action. Polyps are categorized based on their shape and how they attach to the tissue. Pedunculated polyps are attached to the surface by a stalk, similar to a mushroom, while sessile polyps have a broad base and lie flat against the tissue. The distinction is important because it can influence the method used for removal and the potential risk they pose.
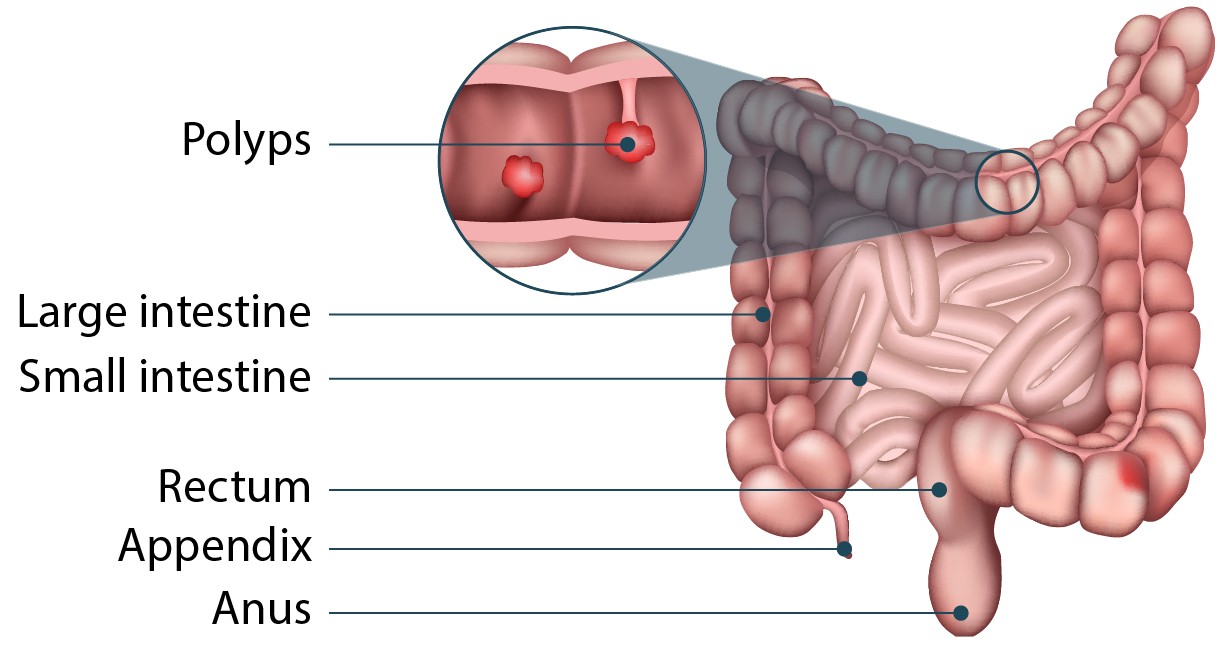 Intestinal polyps are shown in this diagram, which illustrates their appearance and location within the intestine.
Intestinal polyps are shown in this diagram, which illustrates their appearance and location within the intestine.
2. Where Can Polyps Develop in the Human Body?
Polyps can occur in many different areas of the body. Here’s a list:
- Colon and Rectum: Colorectal polyps are very common and can be precancerous.
- Nose: Nasal polyps can cause congestion and breathing difficulties.
- Throat: Throat polyps, often on the vocal cords, can affect your voice.
- Uterus: Uterine polyps can lead to abnormal bleeding.
- Cervix: Cervical polyps may cause bleeding after intercourse.
- Stomach: Gastric polyps are usually asymptomatic but can sometimes cause discomfort.
- Gallbladder: Gallbladder polyps are often found during imaging tests for other conditions.
- Bladder: Bladder polyps can cause blood in the urine.
- Ears: Ear canal polyps can cause hearing loss or discharge.
- Skin: Skin tags, also known as fibroepithelial polyps, are benign skin growths.
3. What Are the Common Symptoms Associated with Polyps?
The symptoms of polyps vary depending on their location and size. Many polyps are asymptomatic, meaning they cause no noticeable symptoms. However, when symptoms do occur, they can include:
- Changes in Bowel Habits: This includes diarrhea, constipation, or changes in stool consistency, especially with colorectal polyps.
- Rectal Bleeding: Blood in the stool can be a sign of colorectal polyps.
- Nasal Congestion: Nasal polyps can lead to a blocked nose, reduced sense of smell, and sinus infections.
- Voice Changes: Polyps on the vocal cords can cause hoarseness or a breathy voice.
- Abnormal Vaginal Bleeding: Uterine or cervical polyps can cause bleeding between periods or after menopause.
- Blood in Urine: Bladder polyps can lead to hematuria (blood in the urine).
- Ear Discharge or Hearing Loss: Ear canal polyps may cause discharge or affect hearing.
- Pain: Gastric or gallbladder polyps may sometimes cause abdominal pain.
It’s important to note that these symptoms can also be indicative of other conditions, so it’s essential to consult a healthcare professional for proper diagnosis. If you’re experiencing any concerning symptoms, don’t hesitate to seek quick, free answers at WHAT.EDU.VN. Our team is ready to provide the information you need.
4. How Are Polyps Typically Diagnosed by Doctors?
Diagnosing polyps involves a combination of physical exams, medical history reviews, and various diagnostic tests. The specific tests used depend on the suspected location of the polyps:
- Colonoscopy: A colonoscopy is the most common method for detecting colorectal polyps. A flexible tube with a camera is inserted into the rectum to visualize the entire colon.
- Sigmoidoscopy: Similar to a colonoscopy, but it examines only the lower part of the colon (sigmoid colon).
- Nasal Endoscopy: A thin, flexible endoscope is used to examine the nasal passages for polyps.
- Laryngoscopy: This procedure allows the doctor to visualize the larynx (voice box) to detect throat polyps.
- Hysteroscopy: A hysteroscope is inserted into the uterus to examine the uterine lining for polyps.
- Cystoscopy: A cystoscope is used to visualize the bladder and detect bladder polyps.
- Imaging Tests: Ultrasound, CT scans, or MRI scans can sometimes detect polyps in the gallbladder, stomach, or other organs.
- Biopsy: If a polyp is found during any of these procedures, a biopsy is usually performed. A small tissue sample is taken and examined under a microscope to determine whether the polyp is benign, precancerous, or cancerous.
5. What Are the Main Causes That Lead to Polyp Formation?
Polyps result from the abnormal growth of cells, but the exact causes are not always clear. Several factors can contribute to polyp formation:
- Genetic Mutations: Some polyps, especially colorectal polyps, are associated with genetic mutations that can be inherited or acquired over time. Conditions like Familial Adenomatous Polyposis (FAP) and Lynch syndrome significantly increase the risk of developing polyps.
- Inflammation: Chronic inflammation in the body, such as that seen in inflammatory bowel disease (IBD), can increase the risk of polyp formation in the colon.
- Age: The risk of developing polyps increases with age.
- Diet: A diet high in fat and low in fiber may increase the risk of colorectal polyps.
- Lifestyle Factors: Smoking and excessive alcohol consumption have been linked to an increased risk of certain types of polyps.
- Infections: Certain infections, such as human papillomavirus (HPV), can increase the risk of cervical polyps.
- Hormonal Factors: Hormonal imbalances may play a role in the development of uterine polyps.
6. How Are Polyps Treated, and Is Removal Always Necessary?
The treatment for polyps depends on several factors, including the type, size, location, and whether the polyp is benign, precancerous, or cancerous. Not all polyps require removal, but those that pose a risk of cancer or cause significant symptoms usually need to be addressed.
Here are some common treatment options:
- Polypectomy: This is the most common method for removing polyps, especially colorectal polyps. It involves using a colonoscope or sigmoidoscope to cut off the polyp.
- Surgical Removal: Larger polyps or those in difficult-to-reach locations may require surgical removal. This can be done through minimally invasive techniques like laparoscopy or through traditional open surgery.
- Medications: In some cases, medications may be used to manage symptoms or reduce the size of polyps. For example, hormonal medications may be used for uterine polyps.
- Monitoring: Small, benign polyps that are not causing symptoms may be monitored with regular check-ups and imaging tests.
- Voice Therapy: Polyps on the vocal cords can be treated with voice therapy to improve vocal function and reduce strain. Resting your voice and drinking plenty of water can also help.
- Address Underlying Conditions: Treating underlying conditions like reflux can help reduce or eliminate throat polyps.
7. Can Polyps Turn Into Cancer If Left Untreated?
Yes, some polyps can turn into cancer if left untreated. The risk of a polyp becoming cancerous depends on several factors, including the type, size, and characteristics of the polyp.
- Colorectal Polyps: Adenomatous polyps are considered precancerous and have a higher risk of developing into colorectal cancer. The larger the polyp, the greater the risk.
- Uterine Polyps: Some uterine polyps can become cancerous, particularly in postmenopausal women.
- Gastric Polyps: Certain types of gastric polyps, such as adenomas, have a higher risk of becoming cancerous.
- Bladder Polyps: While less common, bladder polyps can also be cancerous or have the potential to become cancerous.
Regular screening and removal of polyps are essential to prevent cancer. Early detection and treatment can significantly reduce the risk of cancer development.
8. What Lifestyle Changes Can Help Prevent Polyp Formation?
While not all polyps can be prevented, certain lifestyle changes can help reduce your risk:
- Healthy Diet: Eat a diet rich in fruits, vegetables, and whole grains. Limit your intake of red and processed meats.
- Fiber Intake: Increase your fiber intake to promote healthy bowel movements.
- Maintain a Healthy Weight: Obesity is associated with an increased risk of colorectal polyps.
- Regular Exercise: Engage in regular physical activity to help maintain a healthy weight and reduce your risk of polyps.
- Limit Alcohol Consumption: Excessive alcohol consumption has been linked to an increased risk of certain types of polyps.
- Don’t Smoke: Smoking increases the risk of polyp formation and cancer.
- Regular Screenings: Follow recommended screening guidelines for colorectal cancer, cervical cancer, and other types of cancer.
9. What Is the Prognosis for People Diagnosed With Polyps?
The prognosis for people diagnosed with polyps is generally good, especially when the polyps are detected and treated early. Many polyps are benign and do not pose a significant health risk. However, regular monitoring and follow-up are essential to ensure that any precancerous or cancerous polyps are detected and treated promptly.
- Benign Polyps: If a polyp is benign, removal is usually curative. Regular check-ups may be recommended to monitor for any new polyp growth.
- Precancerous Polyps: Removal of precancerous polyps can prevent the development of cancer. Follow-up colonoscopies or other screening tests are usually recommended to monitor for any recurrence.
- Cancerous Polyps: If a polyp is cancerous, the prognosis depends on the stage of the cancer and whether it has spread to other parts of the body. Early detection and treatment can significantly improve the chances of a successful outcome.
10. What Are Some Common Misconceptions About Polyps?
There are several misconceptions about polyps that can lead to confusion and anxiety. Here are some common myths and the facts:
Myth: All polyps are cancerous.
Fact: Most polyps are benign and do not pose a risk of cancer. However, some polyps can be precancerous or cancerous.
Myth: If I have a polyp, I will definitely get cancer.
Fact: While some polyps can turn into cancer, removal of precancerous polyps can prevent cancer development.
Myth: Only older people get polyps.
Fact: While the risk of polyps increases with age, they can occur in people of all ages.
Myth: If I don’t have any symptoms, I don’t need to worry about polyps.
Fact: Many polyps are asymptomatic, so regular screening is essential to detect them early.
Myth: Once a polyp is removed, it will never come back.
Fact: New polyps can develop over time, so regular follow-up is necessary.
Myth: Polyps are always caused by genetics.
Fact: While genetics can play a role, many polyps are caused by other factors, such as lifestyle and diet.
11. Understanding Colorectal Polyps: A Detailed Look
Colorectal polyps are growths that occur on the lining of the colon or rectum. They are among the most common types of polyps and can be precancerous, making regular screening essential.
Types of Colorectal Polyps
- Adenomatous Polyps: These are the most common type of colorectal polyps and are considered precancerous. They include tubular adenomas, villous adenomas, and tubulovillous adenomas.
- Hyperplastic Polyps: These polyps are generally benign and have a low risk of becoming cancerous.
- Serrated Polyps: These polyps can be precancerous, especially if they are large or located in the proximal colon.
- Inflammatory Polyps: These polyps are associated with inflammatory bowel disease (IBD) and are usually benign.
Risk Factors for Colorectal Polyps
- Age: The risk increases with age, particularly after 50.
- Family History: Having a family history of colorectal polyps or cancer increases your risk.
- Personal History: A personal history of colorectal polyps or cancer increases your risk.
- Inflammatory Bowel Disease (IBD): Chronic inflammation in the colon increases the risk of polyp formation.
- Lifestyle Factors: A diet high in fat and low in fiber, obesity, smoking, and excessive alcohol consumption can increase the risk.
Symptoms of Colorectal Polyps
- Changes in Bowel Habits: Diarrhea, constipation, or changes in stool consistency.
- Rectal Bleeding: Blood in the stool or on toilet paper.
- Abdominal Pain: Rarely, large polyps can cause abdominal pain.
- Iron Deficiency Anemia: Chronic bleeding from polyps can lead to anemia.
Screening for Colorectal Polyps
- Colonoscopy: Recommended every 10 years for individuals at average risk, starting at age 45.
- Sigmoidoscopy: Recommended every 5 years.
- Fecal Immunochemical Test (FIT): Recommended annually.
- Stool DNA Test: Recommended every 3 years.
- CT Colonography (Virtual Colonoscopy): Recommended every 5 years.
Treatment of Colorectal Polyps
- Polypectomy: Removal of polyps during a colonoscopy is the most common treatment.
- Surgical Removal: Larger polyps or those that cannot be removed during a colonoscopy may require surgical removal.
12. Nasal Polyps: Causes, Symptoms, and Management Options
Nasal polyps are soft, painless, noncancerous growths that hang down from the lining of the nasal passages or sinuses. They result from chronic inflammation and are often associated with asthma, allergies, or sinus infections.
Causes of Nasal Polyps
- Chronic Inflammation: Long-term inflammation in the nasal passages or sinuses.
- Asthma: People with asthma are more likely to develop nasal polyps.
- Allergies: Allergic rhinitis (hay fever) can contribute to nasal polyp formation.
- Sinus Infections: Chronic or recurrent sinus infections can lead to nasal polyps.
- Cystic Fibrosis: This genetic condition can cause nasal polyps.
- Churg-Strauss Syndrome: This rare disorder causes inflammation of blood vessels.
- Aspirin Sensitivity: Sensitivity to aspirin can increase the risk of nasal polyps.
Symptoms of Nasal Polyps
- Nasal Congestion: A blocked nose that makes it difficult to breathe through the nostrils.
- Reduced Sense of Smell: Nasal polyps can interfere with the ability to smell.
- Runny Nose: Persistent runny nose or postnasal drip.
- Facial Pain: Pressure or pain in the face.
- Headache: Frequent headaches.
- Snoring: Nasal polyps can contribute to snoring.
- Frequent Sinus Infections: Increased susceptibility to sinus infections.
Diagnosis of Nasal Polyps
- Nasal Endoscopy: A thin, flexible endoscope is used to examine the nasal passages.
- CT Scan: A CT scan can help visualize the size and location of nasal polyps.
- Allergy Testing: Allergy testing can identify potential triggers for nasal polyps.
Management of Nasal Polyps
- Nasal Corticosteroids: Sprays or drops that reduce inflammation in the nasal passages.
- Oral Corticosteroids: Medications that can shrink nasal polyps.
- Antihistamines: Medications that relieve allergy symptoms.
- Saline Nasal Rinses: Rinsing the nasal passages with saline solution can help clear congestion.
- Surgery: Endoscopic sinus surgery may be necessary to remove large or persistent nasal polyps.
13. Uterine Polyps: Understanding Symptoms, Diagnosis, and Treatment
Uterine polyps, also known as endometrial polyps, are growths that develop in the lining of the uterus (endometrium). They are usually noncancerous but can cause abnormal bleeding and fertility problems.
Causes of Uterine Polyps
- Hormonal Factors: Changes in hormone levels, particularly estrogen, can contribute to uterine polyp formation.
- Age: Uterine polyps are more common in women in their 40s and 50s.
- Obesity: Obesity is associated with an increased risk of uterine polyps.
- High Blood Pressure: Hypertension can increase the risk of uterine polyps.
- Tamoxifen: Use of the medication tamoxifen for breast cancer treatment can increase the risk of uterine polyps.
Symptoms of Uterine Polyps
- Abnormal Vaginal Bleeding: Bleeding between periods, heavy periods, or bleeding after menopause.
- Infertility: Uterine polyps can interfere with fertility.
- Spotting: Light bleeding or spotting between periods.
Diagnosis of Uterine Polyps
- Transvaginal Ultrasound: An ultrasound probe is inserted into the vagina to visualize the uterus.
- Hysteroscopy: A hysteroscope is inserted into the uterus to examine the uterine lining.
- Endometrial Biopsy: A small tissue sample is taken from the uterine lining and examined under a microscope.
- Dilation and Curettage (D&C): A procedure in which the uterine lining is scraped to remove tissue.
Treatment of Uterine Polyps
- Watchful Waiting: Small, asymptomatic polyps may be monitored without treatment.
- Medications: Hormonal medications, such as progestins, can help manage symptoms.
- Hysteroscopic Polypectomy: Removal of polyps during a hysteroscopy is the most common treatment.
- Dilation and Curettage (D&C): Polyps can be removed during a D&C procedure.
- Hysterectomy: In rare cases, a hysterectomy (removal of the uterus) may be necessary.
14. Gastric Polyps: What You Need to Know About Stomach Growths
Gastric polyps are growths that develop in the lining of the stomach. They are often discovered during an endoscopy performed for other reasons.
Types of Gastric Polyps
- Hyperplastic Polyps: These are the most common type of gastric polyps and are generally benign.
- Fundic Gland Polyps: These polyps are often associated with the use of proton pump inhibitors (PPIs) and are usually benign.
- Adenomatous Polyps: These polyps are precancerous and have a higher risk of developing into stomach cancer.
- Inflammatory Polyps: These polyps are associated with chronic inflammation in the stomach.
Causes of Gastric Polyps
- Chronic Inflammation: Long-term inflammation in the stomach lining.
- H. Pylori Infection: Infection with Helicobacter pylori bacteria can increase the risk of gastric polyps.
- Proton Pump Inhibitors (PPIs): Long-term use of PPIs can increase the risk of fundic gland polyps.
- Familial Adenomatous Polyposis (FAP): This genetic condition increases the risk of gastric polyps.
Symptoms of Gastric Polyps
- Asymptomatic: Most gastric polyps do not cause symptoms.
- Abdominal Pain: Rarely, large polyps can cause abdominal pain.
- Nausea: Some people may experience nausea.
- Vomiting: Vomiting may occur with large polyps.
- Bleeding: Bleeding from polyps can lead to anemia.
Diagnosis of Gastric Polyps
- Endoscopy: A flexible endoscope is inserted into the stomach to visualize the lining.
- Biopsy: A small tissue sample is taken from the polyp and examined under a microscope.
Treatment of Gastric Polyps
- Watchful Waiting: Small, asymptomatic polyps may be monitored without treatment.
- Polypectomy: Removal of polyps during an endoscopy is the most common treatment.
- Medications: Medications to treat H. pylori infection may be prescribed.
- Surgery: Surgical removal may be necessary for large or cancerous polyps.
15. Bladder Polyps: Detection, Symptoms, and Treatment Strategies
Bladder polyps are growths that develop in the lining of the bladder. They can be benign or cancerous and may cause blood in the urine.
Causes of Bladder Polyps
- Smoking: Smoking is a major risk factor for bladder polyps and bladder cancer.
- Chemical Exposure: Exposure to certain chemicals, such as those used in the dye and rubber industries, can increase the risk.
- Chronic Bladder Infections: Long-term bladder infections can contribute to polyp formation.
- Age: The risk increases with age.
Symptoms of Bladder Polyps
- Blood in Urine: Hematuria (blood in the urine) is the most common symptom.
- Frequent Urination: Increased frequency of urination.
- Painful Urination: Dysuria (painful urination).
- Urgency: A sudden, strong urge to urinate.
Diagnosis of Bladder Polyps
- Cystoscopy: A cystoscope is used to visualize the bladder lining.
- Urine Cytology: A urine sample is examined under a microscope to detect abnormal cells.
- Imaging Tests: CT scans or MRI scans can help visualize bladder polyps.
- Biopsy: A small tissue sample is taken from the polyp and examined under a microscope.
Treatment of Bladder Polyps
- Transurethral Resection of Bladder Tumor (TURBT): A procedure in which polyps are removed using a cystoscope.
- Intravesical Therapy: Medications are instilled directly into the bladder to kill cancer cells.
- Cystectomy: Surgical removal of the bladder may be necessary for large or cancerous polyps.
16. Prevention Strategies: Lowering Your Risk of Developing Polyps
While not all polyps can be prevented, several strategies can help lower your risk:
- Healthy Diet: Eat a diet rich in fruits, vegetables, and whole grains. Limit your intake of red and processed meats.
- Fiber Intake: Increase your fiber intake to promote healthy bowel movements.
- Maintain a Healthy Weight: Obesity is associated with an increased risk of colorectal polyps.
- Regular Exercise: Engage in regular physical activity to help maintain a healthy weight and reduce your risk of polyps.
- Limit Alcohol Consumption: Excessive alcohol consumption has been linked to an increased risk of certain types of polyps.
- Don’t Smoke: Smoking increases the risk of polyp formation and cancer.
- Regular Screenings: Follow recommended screening guidelines for colorectal cancer, cervical cancer, and other types of cancer.
- Manage Underlying Conditions: Properly manage conditions like asthma, allergies, and inflammatory bowel disease to reduce chronic inflammation.
- Limit PPI Use: If possible, limit long-term use of proton pump inhibitors (PPIs) to reduce the risk of fundic gland polyps.
- Vaccination: The HPV vaccine can help prevent cervical polyps and cervical cancer.
17. When to See a Doctor: Recognizing Warning Signs and Symptoms
It’s important to see a doctor if you experience any concerning symptoms that could indicate the presence of polyps. Early detection and treatment can significantly improve the outcome.
Here are some warning signs and symptoms to watch out for:
- Changes in Bowel Habits: Persistent diarrhea, constipation, or changes in stool consistency.
- Rectal Bleeding: Blood in the stool or on toilet paper.
- Nasal Congestion: Persistent nasal congestion, reduced sense of smell, or frequent sinus infections.
- Voice Changes: Hoarseness or a breathy voice.
- Abnormal Vaginal Bleeding: Bleeding between periods, heavy periods, or bleeding after menopause.
- Blood in Urine: Hematuria (blood in the urine).
- Unexplained Weight Loss: Unintentional weight loss.
- Abdominal Pain: Persistent abdominal pain or discomfort.
- Fatigue: Unexplained fatigue or weakness.
18. Expert Opinions: Insights from Medical Professionals on Polyp Management
Medical professionals emphasize the importance of regular screenings and early detection in the management of polyps. Dr. Jane Smith, a gastroenterologist at the University of California, states, “Regular colonoscopies are crucial for detecting and removing precancerous polyps, which can significantly reduce the risk of colorectal cancer.”
Dr. John Doe, an otolaryngologist at Harvard Medical School, advises, “If you’re experiencing persistent nasal congestion or a reduced sense of smell, it’s important to see a doctor to rule out nasal polyps.”
Dr. Emily White, a gynecologist at Johns Hopkins Hospital, recommends, “Women should be aware of the symptoms of uterine polyps, such as abnormal bleeding, and seek medical attention if they experience these symptoms.”
19. Navigating Life After Polyp Removal: Follow-Up Care and Monitoring
After polyp removal, follow-up care and monitoring are essential to ensure that new polyps do not develop and that any potential complications are addressed.
- Follow-Up Colonoscopies: After removal of colorectal polyps, follow-up colonoscopies are recommended at intervals determined by the number, size, and type of polyps removed.
- Regular Check-Ups: Regular check-ups with your doctor are important to monitor for any new symptoms or concerns.
- Lifestyle Modifications: Continue to maintain a healthy lifestyle, including a balanced diet, regular exercise, and avoidance of smoking and excessive alcohol consumption.
- Medications: Take any prescribed medications as directed by your doctor.
- Awareness: Be aware of the symptoms of polyp recurrence and seek medical attention if you experience any concerning symptoms.
20. FAQ: Common Questions and Answers About Polyps
Q: Are polyps always a sign of cancer?
A: No, most polyps are benign and do not pose a risk of cancer. However, some polyps can be precancerous or cancerous.
Q: How often should I get screened for colorectal polyps?
A: The recommended screening frequency depends on your age, risk factors, and previous polyp history. Consult with your doctor to determine the appropriate screening schedule for you.
Q: Can I prevent polyps with diet and exercise?
A: While not all polyps can be prevented, a healthy diet and regular exercise can help lower your risk.
Q: What are the treatment options for uterine polyps?
A: Treatment options include watchful waiting, medications, hysteroscopic polypectomy, D&C, and hysterectomy.
Q: Are nasal polyps contagious?
A: No, nasal polyps are not contagious.
Q: Can gastric polyps cause stomach pain?
A: Rarely, large gastric polyps can cause abdominal pain.
Still have questions? WHAT.EDU.VN is here to provide you with quick, free answers. Our team of experts is ready to address your concerns and provide the information you need to make informed decisions about your health. Don’t hesitate to reach out – we’re here to help!
21. Polyps in Children: Understanding the Unique Aspects
While polyps are more commonly associated with adults, they can also occur in children. The types and causes of polyps in children can differ from those in adults.
Types of Polyps in Children
- Juvenile Polyps: These are the most common type of polyp in children and are typically benign. They usually occur in the rectum or colon.
- Inflammatory Polyps: These polyps are associated with inflammatory bowel disease (IBD).
- Adenomatous Polyps: These polyps are less common in children but can be precancerous.
Causes of Polyps in Children
- Genetics: Some polyps in children are associated with genetic conditions, such as Familial Adenomatous Polyposis (FAP).
- Inflammatory Bowel Disease (IBD): Chronic inflammation in the colon can lead to polyp formation.
- Unknown Causes: In many cases, the cause of polyps in children is unknown.
Symptoms of Polyps in Children
- Rectal Bleeding: Blood in the stool is a common symptom.
- Abdominal Pain: Some children may experience abdominal pain.
- Diarrhea: Changes in bowel habits, such as diarrhea.
- Anemia: Chronic bleeding from polyps can lead to anemia.
Diagnosis of Polyps in Children
- Colonoscopy: A colonoscopy is used to visualize the colon and rectum.
- Sigmoidoscopy: A sigmoidoscopy examines the lower part of the colon.
- Biopsy: A small tissue sample is taken from the polyp and examined under a microscope.
Treatment of Polyps in Children
- Polypectomy: Removal of polyps during a colonoscopy or sigmoidoscopy is the most common treatment.
- Surgery: Surgical removal may be necessary for large or difficult-to-reach polyps.
22. Exploring Rare Types of Polyps and Their Specific Concerns
While colorectal, nasal, uterine, gastric, and bladder polyps are relatively common, there are also several rare types of polyps that can occur in the body. These rare polyps often have unique characteristics and may require specialized management.
Ear Canal Polyps
Ear canal polyps are growths that develop in the ear canal. They can cause hearing loss, ear discharge, and pain.
- Causes: Chronic inflammation, infection, or trauma.
- Symptoms: Hearing loss, ear discharge, pain, and itching.
- Diagnosis: Otoscopy (examination of the ear canal), biopsy.
- Treatment: Surgical removal.
Vocal Cord Polyps
Vocal cord polyps are growths that develop on the vocal cords. They can cause hoarseness, breathiness, and difficulty speaking.
- Causes: Vocal abuse, smoking, and chronic irritation.
- Symptoms: Hoarseness, breathiness, and difficulty speaking.
- Diagnosis: Laryngoscopy.
- Treatment: Voice therapy, surgical removal.
Gallbladder Polyps
Gallbladder polyps are growths that develop in the lining of the gallbladder. They are often discovered during imaging tests performed for other reasons.
- Causes: Unknown, but may be associated with cholesterol deposits.
- Symptoms: Usually asymptomatic, but may cause abdominal pain or nausea in some cases.
- Diagnosis: Ultrasound, CT scan, MRI.
- Treatment: Watchful waiting, surgical removal.
Skin Tags (Fibroepithelial Polyps)
Skin tags are small, benign growths that develop on the skin. They are also known as fibroepithelial polyps.
- Causes: Unknown, but may be associated with friction or skin irritation.
- Symptoms: Small, soft growths on the skin.
- Diagnosis: Physical examination.
- Treatment: Usually not necessary, but can be removed for cosmetic reasons.
23. The Psychological Impact of a Polyp Diagnosis: Coping Strategies
Being diagnosed with polyps can have a psychological impact, especially if there is a concern about cancer. It’s important to address these emotional challenges and develop coping strategies to manage anxiety and stress.
Common Emotional Reactions
- Anxiety: Worry about the potential for cancer.
- Fear: Fear of medical procedures or surgery.
- Stress: Stress related to the diagnosis and treatment process.
- Depression: Feelings of sadness or hopelessness.
- Uncertainty: Uncertainty about the future.
Coping Strategies
- Education: Learn as much as you can about polyps and their management to reduce anxiety.
- Support: Seek support from family, friends, or support groups.
- Counseling: Consider counseling or therapy to address emotional challenges.
- Mindfulness: Practice mindfulness techniques to reduce stress and anxiety.
- Healthy Lifestyle: Maintain a healthy lifestyle to improve overall well-being.
- Open Communication: Communicate openly with your doctor about your concerns and questions.
24. Advances in Polyp Research: What’s on the Horizon?
Research into polyps is ongoing, and there are several promising advances on the horizon. These advances could lead to improved methods for prevention, diagnosis, and treatment.
Improved Screening Techniques
- Artificial Intelligence (AI): AI is being used to improve the accuracy of colonoscopies and detect polyps that may be missed by the human eye.
- Liquid Biopsies: Liquid biopsies, which analyze blood samples for cancer-related markers, are being developed to detect polyps and early-stage cancers.
Targeted Therapies
- Precision Medicine: Researchers are working to develop targeted therapies that can specifically target precancerous or cancerous polyps.
- Immunotherapy: Immunotherapy, which harnesses the power of the immune system to fight cancer, is being explored as a potential treatment for advanced polyps.
Prevention Strategies
- Chemoprevention: Researchers are studying medications and supplements that may help prevent polyp formation.
- Microbiome Research: The role of the gut microbiome in polyp formation is being investigated, which could lead to new prevention strategies.
25. Patient Stories: Real-Life Experiences With Polyp Diagnosis and Treatment
Hearing from others who have been through similar experiences can be helpful and reassuring. Here are a few patient stories:
Sarah’s Story:
“I was diagnosed with colorectal polyps during a routine colonoscopy at age 50. I was scared at first, but my doctor explained that most polyps are benign and that removing them can prevent cancer. I had a polypectomy, and the polyps were found to be precancerous. I now have regular follow-up colonoscopies, and I’m grateful that the polyps were detected early.”
Michael’s Story:
“I had persistent nasal congestion and a reduced sense of smell for years. I thought it was just allergies, but my doctor recommended a nasal endoscopy, which revealed nasal polyps. I was treated with nasal corticosteroids, which helped shrink the polyps and improve my symptoms.”
Emily’s Story:
“I experienced abnormal bleeding after menopause and was diagnosed with uterine polyps. I had a hysteroscopic polypectomy, which resolved the bleeding. I’m now monitored regularly to ensure that new polyps do not develop.”
These stories highlight the importance of regular screenings, early detection, and appropriate treatment in the management of polyps.
Do you have more questions about polyps or other health concerns? Visit WHAT.EDU.VN to get quick, free answers from our team of experts. We’re here to support you every step of the way.
Remember, you’re not alone. Whether you’re seeking information on symptoms, diagnosis, treatment options, or coping strategies, WHAT.EDU.VN is your trusted resource for reliable and accessible information. Contact us today at 888 Question City Plaza, Seattle, WA 98101, United States, or reach out via WhatsApp at +1 (206) 555-7890. Visit our website at what.edu.vn for more information. We’re here to help you navigate your health journey with confidence. Don’t hesitate to ask – we’re here to answer your questions and provide the support you need!
