Are you curious about what an FNP is and what they do? At WHAT.EDU.VN, we provide the answers you need. A family nurse practitioner (FNP) is an advanced practice registered nurse (APRN) specializing in comprehensive healthcare for individuals and families across the lifespan. Explore this in-depth guide to understand the FNP role, its responsibilities, career outlook, and the steps to becoming one, enhancing your understanding of healthcare providers.
1. What Is a Family Nurse Practitioner (FNP)?
What Is An Fnp? An FNP is an advanced practice registered nurse (APRN) focused on providing comprehensive primary care to patients of all ages. FNPs assess, diagnose, and treat a wide range of acute and chronic illnesses, offering patient education and preventive care. They are essential in healthcare, improving patient outcomes and access to care, particularly in underserved areas.
Family nurse practitioners (FNPs) are vital healthcare providers. They are advanced practice registered nurses (APRNs) who provide comprehensive primary care services to patients of all ages, from infants to the elderly. FNPs play a critical role in managing and promoting the health and well-being of individuals and families. The increasing demand for FNPs highlights their significance in the healthcare sector. If you’re seeking reliable information about FNPs and their roles, turn to what.edu.vn for clear and comprehensive answers.
1.1. Key Responsibilities of an FNP
What are the main duties of an FNP? FNPs handle a diverse array of tasks, including physical examinations, ordering and interpreting diagnostic tests, prescribing medications, and developing treatment plans. They also offer counseling and patient education to promote healthy lifestyles. FNPs are often the primary point of contact for patients, emphasizing the importance of preventative care.
FNPs are responsible for a wide array of duties aimed at delivering comprehensive care:
-
Conducting Physical Exams: FNPs perform routine physical examinations to assess the overall health of their patients. This includes checking vital signs, evaluating organ systems, and looking for any signs of illness or disease.
-
Ordering and Interpreting Diagnostic Tests: They order and interpret diagnostic tests such as blood work, X-rays, and other imaging studies. This helps in accurately diagnosing medical conditions.
-
Prescribing Medications: FNPs are authorized to prescribe medications to treat various health conditions. They carefully consider the patient’s medical history, current medications, and potential drug interactions.
-
Developing Treatment Plans: Based on their assessment, FNPs create individualized treatment plans to manage acute and chronic conditions. These plans may include medication, lifestyle modifications, and referrals to specialists.
-
Providing Counseling and Patient Education: FNPs offer counseling and education on healthy lifestyles, disease prevention, and management of chronic conditions. This empowers patients to take an active role in their health.
-
Managing Chronic Diseases: FNPs specialize in the long-term management of chronic diseases like diabetes, hypertension, and asthma. They work with patients to monitor their conditions, adjust treatment plans as needed, and prevent complications.
-
Performing Minor Procedures: FNPs can perform minor procedures such as wound care, vaccinations, and injections.
-
Coordinating Care: FNPs often coordinate patient care with other healthcare professionals, including specialists, therapists, and social workers, to ensure comprehensive and integrated care.
1.2. Importance of FNPs in Healthcare
Why are FNPs vital in healthcare? FNPs expand healthcare access, particularly in rural and underserved areas where physician shortages exist. They offer cost-effective, high-quality care, enhancing patient satisfaction and health outcomes. Their comprehensive approach addresses a wide range of health needs, making them indispensable to modern healthcare systems.
FNPs play a crucial role in the healthcare system for several reasons:
-
Increased Access to Care: FNPs help to bridge the gap in healthcare access, especially in rural and underserved communities where there may be a shortage of physicians. Their presence ensures that more people receive the care they need.
-
Cost-Effective Care: Studies have shown that FNPs provide cost-effective care without compromising quality. Their services often cost less than those provided by physicians for similar health outcomes.
-
High-Quality Care: FNPs are trained to provide comprehensive, patient-centered care. They focus on preventive care and patient education, which leads to better health outcomes.
-
Improved Patient Satisfaction: Patients often report high levels of satisfaction with the care they receive from FNPs. This is due to the holistic approach and the focus on building strong patient-provider relationships.
-
Comprehensive Healthcare: FNPs are trained to manage a wide range of health conditions across the lifespan. This makes them valuable in providing continuous and comprehensive care to individuals and families.
1.3. FNP vs. Other Healthcare Providers
How does an FNP compare to other providers? Compared to physicians, FNPs often emphasize patient education and preventive care. Unlike registered nurses, FNPs can diagnose illnesses, prescribe medications, and manage patient care independently in many states. Compared to specialists, FNPs provide a broader scope of primary care.
Here is a comparison of FNPs with other healthcare providers:
-
FNPs vs. Physicians:
- Similarities: Both FNPs and physicians can diagnose illnesses, prescribe medications, and provide treatment plans.
- Differences: Physicians typically have more specialized training, especially in complex medical cases. FNPs often focus more on patient education and preventive care.
-
FNPs vs. Registered Nurses (RNs):
- Similarities: Both FNPs and RNs provide direct patient care.
- Differences: FNPs have advanced education and training, allowing them to diagnose illnesses and prescribe medications, which RNs cannot do.
-
FNPs vs. Physician Assistants (PAs):
- Similarities: Both FNPs and PAs can diagnose, treat, and prescribe medications under the supervision of a physician (depending on state regulations).
- Differences: FNPs have a nursing background and focus on a holistic, patient-centered approach. PAs are trained in a medical model similar to physicians.
-
FNPs vs. Specialists:
- Similarities: Both FNPs and specialists have in-depth knowledge of specific areas.
- Differences: FNPs provide primary care services and can manage a wide range of health conditions, while specialists focus on a specific area of medicine.
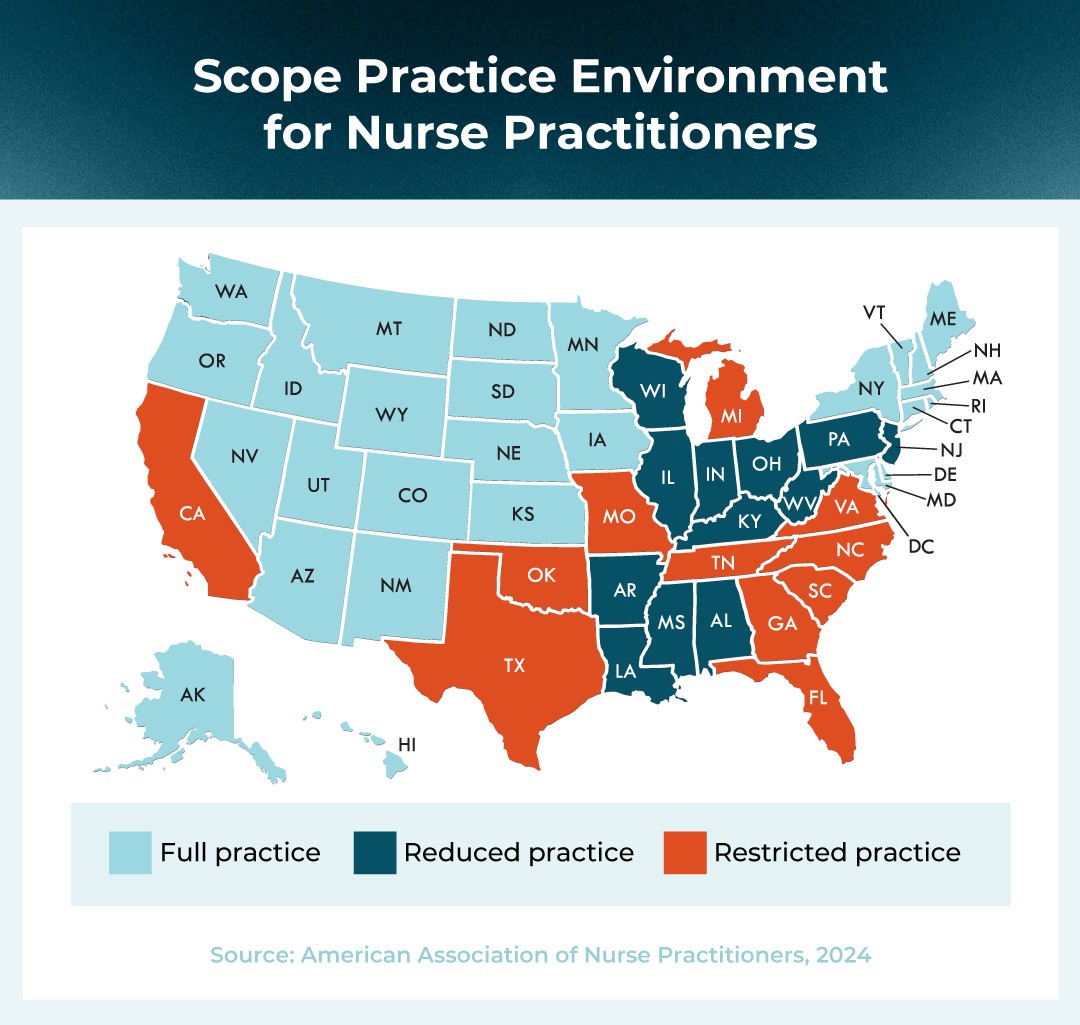
Alt: Scope practice environment illustrating full, reduced, and restricted practice for nurse practitioners across US states.
2. What is an FNP’s Scope of Practice?
What is included in an FNP’s scope? The scope of practice for an FNP varies by state but generally includes diagnosing and treating illnesses, prescribing medications, ordering diagnostic tests, and providing preventive care. In some states, FNPs have full practice authority, allowing them to practice independently.
The scope of practice for family nurse practitioners (FNPs) is broad and comprehensive, enabling them to provide a wide range of healthcare services to patients of all ages. However, it’s important to note that the specific scope of practice can vary depending on state laws and regulations.
2.1. Diagnosing and Treating Illnesses
What can FNPs diagnose and treat? FNPs are qualified to diagnose and treat a wide range of acute and chronic illnesses. This includes common conditions like colds and flu, as well as chronic diseases such as diabetes, hypertension, and heart disease.
FNPs can diagnose and treat a multitude of conditions, including:
- Acute Illnesses: They can diagnose and treat common acute illnesses such as colds, flu, infections, and injuries.
- Chronic Diseases: FNPs manage chronic diseases like diabetes, hypertension, asthma, and arthritis. They develop and implement treatment plans to help patients manage these conditions effectively.
- Mental Health Conditions: Some FNPs are trained to diagnose and manage mental health conditions such as depression and anxiety.
- Women’s Health Issues: FNPs provide care for women’s health issues, including family planning, prenatal care, and menopause management.
- Pediatric Conditions: They also treat common pediatric conditions such as ear infections, asthma, and developmental issues.
2.2. Prescribing Medications
What medications can FNPs prescribe? FNPs can prescribe medications, including controlled substances, in most states. This ability allows them to provide complete treatment plans for their patients.
The authority to prescribe medications is a crucial aspect of an FNP’s scope of practice. In most states, FNPs have the authority to prescribe a wide range of medications, including:
- Prescription Medications: FNPs can prescribe medications to treat various health conditions, including antibiotics, pain relievers, and medications for chronic diseases.
- Controlled Substances: In many states, FNPs can also prescribe controlled substances, which are medications that have a higher potential for abuse or dependence.
- Medical Devices: FNPs can prescribe medical devices such as insulin pumps, nebulizers, and other equipment needed for patient care.
2.3. Ordering and Interpreting Diagnostic Tests
Why is ordering tests part of FNP work? FNPs can order and interpret diagnostic tests such as blood tests, X-rays, and other imaging studies. This helps them accurately diagnose medical conditions and monitor the effectiveness of treatment plans.
The ability to order and interpret diagnostic tests is essential for FNPs to provide comprehensive care. This includes:
- Laboratory Tests: FNPs can order blood tests, urine tests, and other lab tests to assess a patient’s health and diagnose medical conditions.
- Imaging Studies: They can order X-rays, CT scans, MRIs, and other imaging studies to evaluate internal organs and structures.
- Cardiac Tests: FNPs can order electrocardiograms (ECGs) and other cardiac tests to assess heart function.
- Pulmonary Function Tests: They can order pulmonary function tests to evaluate lung function.
2.4. Providing Preventive Care
What preventive services do FNPs provide? FNPs offer a variety of preventive services, including vaccinations, screenings, and health education. This focus on prevention helps patients maintain their health and avoid future medical problems.
FNPs place a strong emphasis on preventive care to help patients stay healthy and prevent illness. Preventive services include:
- Vaccinations: FNPs administer vaccinations to protect against infectious diseases such as influenza, pneumonia, and measles.
- Screenings: They perform screenings for common conditions such as cancer, diabetes, and high blood pressure.
- Health Education: FNPs provide education on healthy lifestyles, including diet, exercise, and stress management.
- Well-Child Visits: They conduct well-child visits to monitor growth and development and provide vaccinations.
- Annual Physical Exams: FNPs perform annual physical exams to assess overall health and identify potential health problems.
2.5. Full Practice Authority
What does full practice mean for FNPs? In states with full practice authority, FNPs can practice independently without physician oversight. This allows them to open their own clinics and provide care directly to patients.
Full practice authority (FPA) grants FNPs the ability to practice to the full extent of their education and training, without the supervision or collaboration of a physician. This includes:
- Independent Practice: FNPs can practice independently, without the need for a collaborative agreement with a physician.
- Opening Own Clinics: They can open and manage their own clinics and healthcare practices.
- Hospital Privileges: FNPs can obtain hospital privileges, allowing them to admit and care for patients in the hospital setting.
- Prescribing Authority: They have full prescribing authority, including the ability to prescribe controlled substances.
Alt: Rising demand for nurse practitioners is visually represented in a bar graph, showing substantial growth.
3. What is the FNP’s Role in Different Healthcare Settings?
Where do FNPs work? FNPs work in various healthcare settings, including primary care clinics, hospitals, urgent care centers, schools, and private practices. Their versatility allows them to address diverse healthcare needs across different environments.
Family Nurse Practitioners (FNPs) are versatile healthcare providers who can work in a variety of settings. Their broad scope of practice and comprehensive training make them valuable assets in numerous healthcare environments.
3.1. Primary Care Clinics
What do FNPs do in clinics? In primary care clinics, FNPs provide routine check-ups, manage chronic conditions, and treat acute illnesses. They serve as primary healthcare providers for many individuals and families.
Primary care clinics are one of the most common settings for FNPs. In this role, they:
- Provide Routine Check-ups: FNPs conduct regular check-ups to monitor patients’ health and identify potential problems early.
- Manage Chronic Conditions: They manage chronic conditions such as diabetes, hypertension, and asthma, helping patients maintain their health and prevent complications.
- Treat Acute Illnesses: FNPs diagnose and treat acute illnesses such as colds, flu, and infections.
- Offer Preventive Care: They offer preventive care services such as vaccinations and screenings.
- Serve as Primary Healthcare Providers: Many individuals and families rely on FNPs as their primary healthcare providers, entrusting them with their overall health and well-being.
3.2. Hospitals
What is an FNP’s responsibility in hospitals? In hospitals, FNPs work in various departments, including emergency rooms, medical-surgical units, and specialty clinics. They assist in patient assessment, treatment, and management, often collaborating with physicians and other healthcare professionals.
In hospitals, FNPs work as part of a multidisciplinary team to provide comprehensive patient care. Their responsibilities include:
- Assisting in Patient Assessment: FNPs conduct patient assessments, including reviewing medical history, performing physical exams, and ordering diagnostic tests.
- Developing Treatment Plans: They collaborate with physicians and other healthcare professionals to develop and implement treatment plans.
- Managing Patient Care: FNPs manage patient care, including monitoring vital signs, administering medications, and providing patient education.
- Working in Various Departments: They work in various hospital departments, including emergency rooms, medical-surgical units, and specialty clinics.
3.3. Urgent Care Centers
How do FNPs help in urgent care? In urgent care centers, FNPs treat patients with acute illnesses and injuries that require immediate attention but are not life-threatening. They provide quick and efficient care to address patients’ urgent healthcare needs.
Urgent care centers provide immediate care for patients with acute illnesses and injuries. FNPs in this setting:
- Treat Acute Illnesses and Injuries: They treat patients with conditions such as colds, flu, minor cuts, and sprains.
- Provide Quick and Efficient Care: FNPs provide quick and efficient care to address patients’ urgent healthcare needs.
- Order Diagnostic Tests: They order diagnostic tests such as X-rays and lab tests to help diagnose medical conditions.
- Prescribe Medications: FNPs prescribe medications to treat various illnesses and injuries.
3.4. Schools
Why are FNPs needed in schools? In schools, FNPs provide healthcare services to students and staff. They conduct physical exams, treat minor injuries and illnesses, and offer health education to promote wellness among the school community.
FNPs play a crucial role in promoting the health and well-being of students and staff in schools. Their responsibilities include:
- Conducting Physical Exams: FNPs conduct physical exams to ensure students are healthy and fit for school activities.
- Treating Minor Injuries and Illnesses: They treat minor injuries and illnesses that occur at school.
- Providing Health Education: FNPs offer health education to students and staff on topics such as nutrition, hygiene, and disease prevention.
- Managing Chronic Conditions: They help manage chronic conditions such as asthma and diabetes among students.
3.5. Private Practices
What does an FNP do in private practice? In private practices, FNPs may work independently or in collaboration with physicians. They provide comprehensive primary care services to their patients, building long-term relationships and managing their health over time.
In private practices, FNPs have the opportunity to provide comprehensive primary care services and build long-term relationships with their patients. Their responsibilities include:
- Providing Comprehensive Primary Care: FNPs provide a wide range of primary care services, including routine check-ups, chronic disease management, and acute illness treatment.
- Building Long-Term Relationships: They build long-term relationships with their patients, providing personalized care and support over time.
- Working Independently or Collaboratively: FNPs may work independently or in collaboration with physicians, depending on state regulations and the practice setting.
- Managing Patient Health: They manage patient health by providing preventive care, diagnosing and treating illnesses, and coordinating care with specialists as needed.
Alt: Shield icon with text “Want to know more about our nursing programs?” linking to program information and a request form.
4. What is FNP Education and Training?
What education do FNPs need? To become an FNP, one must complete a Bachelor of Science in Nursing (BSN), followed by a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP) program with a focus on family practice. Certification is required after graduation.
Family Nurse Practitioners (FNPs) undergo extensive education and training to equip them with the knowledge and skills necessary to provide comprehensive primary care to patients of all ages.
4.1. Bachelor of Science in Nursing (BSN)
Why start with a BSN? The first step is earning a BSN, which provides a solid foundation in nursing principles and practice. This degree covers essential topics such as anatomy, physiology, pharmacology, and patient care.
A Bachelor of Science in Nursing (BSN) is the foundational degree for aspiring FNPs. It provides a comprehensive education in nursing principles and practice, including:
- Core Nursing Courses: The curriculum includes courses in anatomy, physiology, microbiology, pharmacology, and nutrition.
- Clinical Rotations: Students participate in clinical rotations in various healthcare settings, such as hospitals, clinics, and long-term care facilities.
- Patient Care Skills: They learn essential patient care skills, including assessment, medication administration, wound care, and patient education.
- Leadership and Management: The BSN program also covers leadership and management principles, preparing nurses to take on leadership roles in healthcare.
4.2. Master of Science in Nursing (MSN) or Doctor of Nursing Practice (DNP)
How important is graduate study for FNPs? After the BSN, nurses pursue an MSN or DNP with a specialization in family practice. These advanced programs provide in-depth knowledge of advanced assessment, diagnosis, and treatment of illnesses.
After completing a BSN, nurses pursue a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP) degree with a specialization in family practice. These advanced programs:
- Advanced Coursework: The curriculum includes advanced coursework in areas such as advanced pathophysiology, pharmacology, and health assessment.
- Clinical Practicum: Students complete a significant number of clinical hours under the supervision of experienced FNPs and physicians.
- Specialized Knowledge: They gain specialized knowledge in areas such as chronic disease management, women’s health, pediatrics, and geriatrics.
- Leadership Skills: MSN and DNP programs also focus on developing leadership skills, preparing graduates to lead healthcare teams and improve patient outcomes.
4.3. FNP Certification
Why is certification necessary? After completing their graduate program, FNPs must pass a national certification exam to become licensed. This certification ensures they have met the required standards of knowledge and competence.
Certification is a critical step for FNPs, ensuring they have met the required standards of knowledge and competence to practice. The certification process includes:
- National Certification Exam: Graduates must pass a national certification exam administered by organizations such as the American Academy of Nurse Practitioners Certification Board (AANPCB) or the American Nurses Credentialing Center (ANCC).
- Continuing Education: FNPs must maintain their certification by completing continuing education requirements throughout their careers.
- Renewal Requirements: Certification must be renewed periodically, typically every five years, to ensure FNPs stay current with the latest advances in healthcare.
4.4. Continuing Education
How do FNPs stay current? FNPs participate in continuing education activities throughout their careers to stay updated on the latest medical advancements and best practices. This ongoing learning ensures they provide the best possible care to their patients.
Continuing education is essential for FNPs to stay current with the latest medical advancements and best practices. This includes:
- Conferences and Workshops: FNPs attend conferences and workshops to learn about new research, treatment guidelines, and technologies.
- Online Courses: They take online courses to expand their knowledge in specific areas of interest.
- Professional Journals: FNPs read professional journals to stay informed about the latest developments in healthcare.
- Clinical Practice: They gain new knowledge and skills through their daily clinical practice.
4.5. Skills and Competencies
What skills define a good FNP? Effective FNPs possess strong clinical skills, excellent communication skills, and the ability to empathize with patients. They are critical thinkers and problem-solvers, capable of making informed decisions in complex situations.
Effective FNPs possess a range of skills and competencies that enable them to provide high-quality care to their patients. These include:
- Clinical Skills: FNPs have strong clinical skills in areas such as physical assessment, diagnosis, and treatment.
- Communication Skills: They have excellent communication skills, enabling them to effectively communicate with patients, families, and other healthcare professionals.
- Empathy: FNPs are empathetic and compassionate, providing emotional support to patients and their families.
- Critical Thinking: They are critical thinkers and problem-solvers, capable of making informed decisions in complex situations.
- Cultural Competence: FNPs are culturally competent, understanding and respecting the cultural beliefs and values of their patients.
Alt: A family nurse practitioner (FNP) is consulting with an older female patient.
5. What is the FNP Career Outlook and Salary?
What are the job prospects for FNPs? The career outlook for FNPs is excellent, with a projected growth rate much faster than the average for all occupations. The demand for FNPs is driven by the increasing need for primary care services, particularly in underserved areas.
The career outlook for Family Nurse Practitioners (FNPs) is exceptionally promising. The demand for FNPs is driven by several factors, including the increasing need for primary care services, the aging population, and the shortage of physicians in many areas.
5.1. Job Growth
How fast is the FNP field growing? The job market for FNPs is expected to grow significantly over the next decade. This growth is fueled by the rising demand for healthcare services and the increasing recognition of FNPs as valuable members of the healthcare team.
The job market for FNPs is projected to grow substantially in the coming years. According to the U.S. Bureau of Labor Statistics:
- Projected Growth Rate: The employment of nurse practitioners, including FNPs, is projected to grow 46% from 2021 to 2031, much faster than the average for all occupations.
- New Job Openings: This growth is expected to result in approximately 114,900 new job openings over the decade.
- Factors Driving Growth: The increasing demand for healthcare services, the aging population, and the shortage of primary care physicians are driving this growth.
5.2. Average Salary
What is an FNP’s earning potential? The average salary for FNPs is competitive and varies depending on factors such as location, experience, and practice setting. FNPs generally earn higher salaries than registered nurses due to their advanced education and training.
The average salary for FNPs is competitive and varies depending on several factors. According to the U.S. Bureau of Labor Statistics:
- Median Annual Wage: The median annual wage for nurse practitioners was $123,780 in May 2021.
- Salary Range: The salary range for FNPs can vary widely, with the lowest 10 percent earning less than $86,740 and the highest 10 percent earning more than $195,490.
- Factors Affecting Salary: Factors such as location, experience, education, and practice setting can influence an FNP’s salary.
5.3. Factors Influencing Salary
What affects FNP pay? Several factors can influence an FNP’s salary, including geographic location, years of experience, level of education, and the type of healthcare setting in which they work.
Several factors can influence an FNP’s salary:
- Geographic Location: Salaries for FNPs tend to be higher in metropolitan areas and regions with a high cost of living.
- Experience: FNPs with more years of experience typically earn higher salaries.
- Education: FNPs with a Doctor of Nursing Practice (DNP) degree may earn more than those with a Master of Science in Nursing (MSN) degree.
- Practice Setting: Salaries can vary depending on the practice setting, with FNPs working in hospitals and specialty clinics often earning more than those in primary care clinics.
- Demand: Areas with a high demand for FNPs may offer higher salaries to attract qualified candidates.
5.4. Job Security
How stable is the FNP career? FNPs enjoy high job security due to the increasing demand for their services. Their ability to provide cost-effective, high-quality care makes them essential in the healthcare system.
FNPs enjoy high job security due to the increasing demand for their services. Their ability to provide cost-effective, high-quality care makes them essential in the healthcare system.
- High Demand: The demand for FNPs is projected to continue to grow in the coming years, ensuring job security for those in the profession.
- Versatile Skill Set: FNPs have a versatile skill set that allows them to work in a variety of healthcare settings, providing flexibility and job opportunities.
- Essential Role: They play an essential role in the healthcare system, particularly in primary care and underserved areas, making them valuable and sought-after healthcare providers.
5.5. Career Advancement
What are FNP career options? FNPs have opportunities for career advancement, such as specializing in a particular area of practice, becoming a clinical preceptor for students, or pursuing leadership roles in healthcare organizations.
FNPs have numerous opportunities for career advancement. These include:
- Specialization: FNPs can specialize in a particular area of practice, such as cardiology, dermatology, or oncology, by obtaining additional education and certification.
- Clinical Preceptor: They can become clinical preceptors for nursing students, mentoring and guiding the next generation of healthcare providers.
- Leadership Roles: FNPs can pursue leadership roles in healthcare organizations, such as nurse manager, director of nursing, or chief nursing officer.
- Entrepreneurship: Some FNPs choose to open their own clinics or healthcare practices, providing primary care services to their communities.
- Research: FNPs can engage in research to advance nursing knowledge and improve patient outcomes.
6. What Are the Pros and Cons of Being an FNP?
Is being an FNP a good fit? Being an FNP offers many rewards, including the opportunity to make a significant impact on patients’ lives and enjoy a flexible career. However, it also presents challenges such as dealing with high stress levels and managing complex medical cases.
Becoming a Family Nurse Practitioner (FNP) is a rewarding but demanding career path. It offers numerous benefits, but also comes with its share of challenges.
6.1. Pros of Being an FNP
What are the advantages of being an FNP?
- High Demand and Job Security: FNPs are in high demand, ensuring job security and career opportunities.
- Competitive Salary: FNPs earn competitive salaries, reflecting their advanced education and training.
- Making a Difference: FNPs have the opportunity to make a significant impact on patients’ lives by providing comprehensive primary care.
- Autonomy and Independence: FNPs enjoy a high degree of autonomy and independence, particularly in states with full practice authority.
- Flexible Career Options: FNPs can work in a variety of healthcare settings and specialize in different areas of practice.
Being an FNP offers numerous advantages that make it a fulfilling and rewarding career:
- High Demand and Job Security: The demand for FNPs is growing rapidly, ensuring job security and numerous career opportunities.
- Competitive Salary: FNPs earn competitive salaries that reflect their advanced education, training, and responsibilities.
- Making a Difference: FNPs have the opportunity to make a significant impact on the lives of their patients by providing comprehensive primary care.
- Autonomy and Independence: In many states, FNPs have a high degree of autonomy and can practice independently without physician supervision.
- Flexible Career Options: FNPs can work in a variety of settings, including clinics, hospitals, schools, and private practices, allowing for flexible career options.
- Professional Growth: There are ample opportunities for professional growth and specialization within the FNP field.
6.2. Cons of Being an FNP
What are the challenges FNPs face?
- High Stress Levels: FNPs often work in fast-paced environments and deal with high-stress situations.
- Long Hours: FNPs may work long and irregular hours, including weekends and holidays.
- Emotional Toll: FNPs may experience emotional toll from dealing with patients’ illnesses and suffering.
- Administrative Burden: FNPs may face administrative burden related to paperwork, billing, and insurance.
- Scope of Practice Restrictions: In some states, FNPs face restrictions on their scope of practice, limiting their autonomy and ability to provide care.
Despite the many benefits, there are also challenges to consider when pursuing a career as an FNP:
- High Stress Levels: The fast-paced and demanding nature of healthcare can lead to high levels of stress.
- Long and Irregular Hours: FNPs often work long and irregular hours, including weekends and holidays.
- Emotional Toll: Dealing with sick and suffering patients can take an emotional toll.
- Administrative Burden: Like many healthcare professionals, FNPs face administrative tasks such as paperwork, billing, and insurance-related issues.
- Scope of Practice Restrictions: In some states, FNPs have limited scope of practice and must work under the supervision of a physician.
6.3. Balancing Pros and Cons
How do you decide if FNP is right for you? Deciding whether to become an FNP involves weighing the pros and cons and considering your personal and professional goals. If you are passionate about primary care, enjoy working with patients of all ages, and are willing to take on the challenges of the profession, then being an FNP may be a rewarding career choice.
To determine if becoming an FNP is the right career path for you, carefully consider the pros and cons. Reflect on your personal and professional goals, interests, and strengths. If you are passionate about primary care, enjoy working with patients of all ages, and are prepared to handle the challenges, then a career as an FNP can be highly fulfilling.
Alt: A colorful map detailing the scope of practice environment for nurse practitioners across the United States.
7. What are Some Common FNP Specialties?
Are there FNP subspecialties? While family practice is a broad specialty, FNPs can further specialize in areas such as women’s health, pediatrics, geriatrics, or mental health.
While Family Nurse Practitioners (FNPs) are trained to provide comprehensive care across the lifespan, many choose to specialize further in specific areas of healthcare.
7.1. Women’s Health
What does women’s health FNP care entail? FNPs specializing in women’s health provide care related to reproductive health, prenatal care, and menopause management.
FNPs specializing in women’s health focus on the unique healthcare needs of women, including:
- Reproductive Health: Providing care related to contraception, family planning, and fertility issues.
- Prenatal Care: Offering care and support during pregnancy, including prenatal check-ups, education, and monitoring.
- Menopause Management: Helping women manage the symptoms of menopause, such as hot flashes, mood swings, and sleep disturbances.
- Gynecological Care: Performing routine gynecological exams, Pap smears, and screenings for sexually transmitted infections (STIs).
- Breast Health: Providing education and screening for breast cancer and other breast-related conditions.
7.2. Pediatrics
What do pediatric FNPs focus on? FNPs specializing in pediatrics focus on the healthcare needs of infants, children, and adolescents. They provide well-child exams, vaccinations, and treatment for common childhood illnesses.
FNPs specializing in pediatrics are dedicated to the health and well-being of infants, children, and adolescents:
- Well-Child Exams: Conducting routine check-ups to monitor growth and development, administer vaccinations, and provide anticipatory guidance.
- Acute Illness Management: Diagnosing and treating common childhood illnesses such as ear infections, colds, and flu.
- Chronic Disease Management: Helping children and adolescents manage chronic conditions such as asthma, diabetes, and allergies.
- Developmental Screening: Assessing children for developmental delays and providing referrals for early intervention services.
- Adolescent Health: Addressing the unique healthcare needs of adolescents, including reproductive health, mental health, and substance abuse prevention.
7.3. Geriatrics
What kind of care do geriatric FNPs give? FNPs specializing in geriatrics provide care to older adults, focusing on managing chronic conditions, promoting healthy aging, and addressing age-related health issues.
FNPs specializing in geriatrics provide comprehensive care to older adults, focusing on:
- Chronic Disease Management: Helping older adults manage chronic conditions such as arthritis, heart disease, and dementia.
- Medication Management: Reviewing and managing medications to minimize side effects and drug interactions.
- Preventive Care: Providing preventive services such as vaccinations, screenings, and fall prevention strategies.
- Geriatric Assessment: Conducting comprehensive geriatric assessments to evaluate physical, cognitive, and functional health.
- End-of-Life Care: Offering compassionate end-of-life care and support to patients and their families.
7.4. Mental Health
How do FNPs address mental health? FNPs specializing in mental health provide assessment, diagnosis, and treatment of mental health conditions. They offer therapy, prescribe medications, and provide support to individuals with mental health disorders.
FNPs specializing in mental health, also known as Psychiatric Mental Health Nurse Practitioners (PMHNPs), provide comprehensive mental healthcare services:
- Assessment and Diagnosis: Conducting thorough assessments to diagnose mental health conditions such as depression, anxiety, bipolar disorder, and schizophrenia.
- Medication Management: Prescribing and managing psychiatric medications to alleviate symptoms and improve mental health.
- Therapy: Providing individual, group, and family therapy to address emotional and behavioral issues.
- Crisis Intervention: Offering crisis intervention services to individuals experiencing acute mental health crises.
- Consultation and Collaboration: Collaborating with other healthcare professionals to provide integrated mental healthcare services.
7.5. Other Specialties
Are there other FNP specializations? Other potential FNP specialties include:
- Oncology: Providing care to cancer patients, including chemotherapy administration and symptom management.
- Cardiology: Managing patients with heart conditions and providing preventive cardiology services.
- Dermatology: Treating skin conditions and providing dermatological care.
- Emergency Medicine: Working in emergency departments to provide acute care services.
Alt: A bar graph illustrating the rising demand for nurse practitioners in the healthcare sector.
8. How to Find a Qualified FNP?
How can I locate a good FNP? Finding a qualified FNP involves checking their credentials, considering their experience, and reading patient reviews. You can ask for referrals from your primary care physician or use online directories to find FNPs in your area.
Finding a qualified Family Nurse Practitioner (FNP) involves several steps to ensure you receive the best possible care