Barrett’s esophagus is a condition where the lining of your esophagus changes, often due to acid reflux, and WHAT.EDU.VN can help you understand this condition better. It’s crucial to understand the causes, symptoms, and treatment options. Learn about esophageal cancer risk and preventative measures for Barrett’s esophagus and GERD.
1. What Is Barrett’s Esophagus?
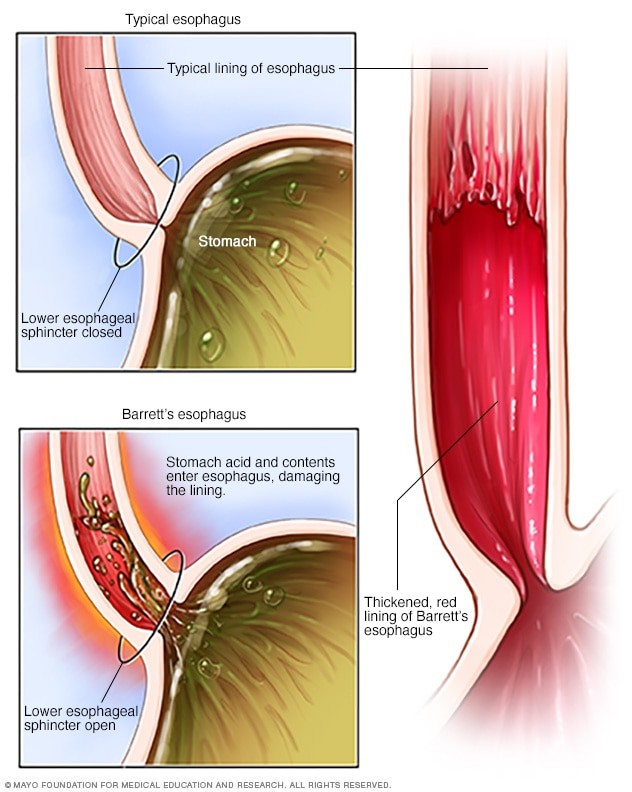
Barrett’s esophagus is a medical condition in which the normal, flat, pink lining of the esophagus (the tube that carries food from the mouth to the stomach) is replaced by tissue that is similar to the lining of the intestine. This change is usually a result of long-term exposure to stomach acid. Over time, this acid damages the esophagus, leading to the development of specialized intestinal metaplasia, the hallmark of Barrett’s esophagus.
To elaborate:
- Esophagus: The muscular tube connecting the throat to the stomach.
- Lining: The inner layer of cells protecting the esophagus.
- Metaplasia: The abnormal change in the nature of a tissue.
- Intestinal Metaplasia: The presence of intestinal-like cells in the esophageal lining.
This condition is important because it increases the risk of developing esophageal adenocarcinoma, a type of esophageal cancer. However, the risk of cancer is relatively low, and regular monitoring can help detect any precancerous changes early.
2. What Are The Main Causes Of Barrett’s Esophagus?
The primary cause of Barrett’s esophagus is chronic gastroesophageal reflux disease (GERD). GERD occurs when stomach acid frequently flows back into the esophagus, irritating and damaging its lining. While GERD is a major risk factor, not everyone with GERD develops Barrett’s esophagus. Some individuals may have what’s known as “silent reflux,” where they experience little to no noticeable GERD symptoms.
Other contributing factors include:
- Long-Term GERD: Prolonged exposure to stomach acid.
- Hiatal Hernia: A condition where the upper part of the stomach bulges through the diaphragm.
- Obesity: Excess weight can increase abdominal pressure, leading to acid reflux.
- Smoking: Tobacco use can weaken the lower esophageal sphincter (LES), allowing acid to escape into the esophagus.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the exact mechanism by which GERD leads to Barrett’s esophagus is not fully understood, but it is believed that the constant irritation and inflammation play a significant role.
3. What Are The Common Symptoms Of Barrett’s Esophagus?
Many people with Barrett’s esophagus don’t experience any symptoms at all. For those who do, the symptoms are often similar to those of GERD.
Common symptoms include:
- Frequent Heartburn: A burning sensation in the chest, often after eating.
- Regurgitation: The sensation of stomach contents flowing back up into the mouth or esophagus.
- Difficulty Swallowing (Dysphagia): A feeling that food is getting stuck in the esophagus.
- Chest Pain: Although less common, some individuals may experience chest pain.
- Hoarseness: Acid reflux can irritate the vocal cords, leading to hoarseness.
- Chronic Cough: Persistent coughing, especially at night.
It’s important to note that the absence of symptoms doesn’t rule out the presence of Barrett’s esophagus. Regular check-ups are crucial, especially for those with long-standing GERD.
4. How Is Barrett’s Esophagus Diagnosed?
Barrett’s esophagus is typically diagnosed through an upper endoscopy. During this procedure, a gastroenterologist inserts a long, flexible tube with a camera attached (endoscope) into the esophagus. This allows the doctor to visually inspect the lining of the esophagus and identify any abnormal changes.
The key steps in diagnosis include:
- Endoscopy: Visual examination of the esophagus.
- Biopsy: Taking small tissue samples from the esophagus lining for microscopic examination.
- Pathology: Analysis of the tissue samples to confirm the presence of Barrett’s esophagus and check for dysplasia (precancerous changes).
According to the American Society for Gastrointestinal Endoscopy (ASGE), the presence of specialized intestinal metaplasia in the biopsy samples is required for a definitive diagnosis of Barrett’s esophagus.
5. What Is Dysplasia In The Context Of Barrett’s Esophagus?
Dysplasia refers to the presence of abnormal cells within the Barrett’s esophagus tissue. It is considered a precancerous condition, meaning that these cells have the potential to develop into cancer over time. Dysplasia is categorized into two main grades:
- Low-Grade Dysplasia: Indicates early precancerous changes.
- High-Grade Dysplasia: Indicates more advanced precancerous changes with a higher risk of progressing to cancer.
The management of dysplasia depends on the grade and extent of the abnormal cells. Regular surveillance and treatment options are crucial in preventing the progression to esophageal cancer.
6. What Are The Treatment Options For Barrett’s Esophagus?
The treatment for Barrett’s esophagus varies depending on whether dysplasia is present and its grade. Treatment strategies aim to manage symptoms, prevent progression to cancer, and improve overall esophageal health.
Common treatment options include:
- Acid Suppression Medications: Proton pump inhibitors (PPIs) are commonly prescribed to reduce stomach acid production.
- Endoscopic Surveillance: Regular endoscopies with biopsies to monitor for any changes in the esophageal lining.
- Endoscopic Resection: Removal of abnormal tissue using endoscopic techniques.
- Radiofrequency Ablation (RFA): Using radiofrequency energy to destroy abnormal cells.
- Photodynamic Therapy (PDT): Using a light-sensitive drug and laser to destroy abnormal cells.
- Surgery: In severe cases, surgical removal of the affected portion of the esophagus may be necessary.
According to Mayo Clinic, the specific treatment plan is tailored to the individual’s condition and risk factors.
7. How Can Lifestyle Changes Help Manage Barrett’s Esophagus?
Lifestyle changes can play a significant role in managing Barrett’s esophagus and reducing symptoms. These changes primarily focus on reducing acid reflux and promoting overall esophageal health.
Key lifestyle modifications include:
- Weight Management: Losing weight if overweight or obese can reduce abdominal pressure and decrease acid reflux.
- Dietary Changes: Avoiding foods that trigger acid reflux, such as fatty foods, spicy foods, chocolate, caffeine, and alcohol.
- Smaller, More Frequent Meals: Eating smaller meals more frequently can reduce the amount of acid produced at any one time.
- Avoid Eating Before Bed: Not eating at least 2-3 hours before lying down can prevent nighttime acid reflux.
- Elevate Head of Bed: Raising the head of the bed by 6-8 inches can help prevent acid from flowing back into the esophagus during sleep.
- Quit Smoking: Smoking weakens the LES and increases acid production.
The American College of Gastroenterology recommends these lifestyle modifications as an integral part of managing GERD and Barrett’s esophagus.
8. What Is The Connection Between Barrett’s Esophagus And Esophageal Cancer?
Barrett’s esophagus is a significant risk factor for esophageal adenocarcinoma, a type of cancer that develops in the lining of the esophagus. The risk of developing cancer is higher in individuals with Barrett’s esophagus compared to the general population.
Key points about the connection include:
- Increased Risk: Barrett’s esophagus increases the risk of esophageal adenocarcinoma.
- Dysplasia Progression: Dysplasia (precancerous changes) in Barrett’s esophagus can progress to cancer over time.
- Surveillance: Regular surveillance with endoscopy and biopsy is crucial to detect and manage dysplasia.
- Early Detection: Early detection and treatment of dysplasia can prevent the development of esophageal cancer.
According to research published in Gastrointestinal Endoscopy, the annual risk of esophageal cancer in individuals with Barrett’s esophagus is approximately 0.5%.
9. How Often Should Someone With Barrett’s Esophagus Undergo Surveillance?
The frequency of surveillance endoscopies for Barrett’s esophagus depends on the presence and grade of dysplasia. The goal of surveillance is to detect any precancerous changes early, allowing for timely intervention.
General guidelines include:
- No Dysplasia: Surveillance endoscopy every 3-5 years.
- Low-Grade Dysplasia: Surveillance endoscopy every 6-12 months.
- High-Grade Dysplasia: More frequent surveillance or treatment options such as endoscopic resection or ablation.
The American Gastroenterological Association (AGA) provides detailed guidelines on the surveillance and management of Barrett’s esophagus.
10. What Are The Latest Advances In Barrett’s Esophagus Treatment?
Several advancements have been made in the treatment of Barrett’s esophagus in recent years. These advancements focus on improving detection, treatment efficacy, and patient outcomes.
Notable advances include:
- High-Resolution Endoscopy: Enhanced imaging techniques to improve the detection of dysplasia.
- Confocal Endomicroscopy: Provides real-time microscopic imaging of the esophageal lining during endoscopy.
- Volumetric Laser Endomicroscopy: Creates three-dimensional images of the esophageal lining to detect abnormalities.
- Cryoablation: Using extreme cold to destroy abnormal cells.
- Improved RFA Techniques: Enhanced radiofrequency ablation methods for more effective treatment.
According to a review in Mayo Clinic Proceedings, these advancements have significantly improved the management and outcomes for individuals with Barrett’s esophagus.
11. Can Medications Help Manage Barrett’s Esophagus?
Yes, medications play a crucial role in managing Barrett’s esophagus, primarily by reducing stomach acid and alleviating symptoms. The most common type of medication prescribed is proton pump inhibitors (PPIs).
- Proton Pump Inhibitors (PPIs): These medications reduce the production of stomach acid, providing relief from heartburn and other GERD symptoms.
- H2 Blockers: These medications also reduce stomach acid production, but are generally less potent than PPIs.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), PPIs are the most effective medications for managing GERD and reducing the risk of complications associated with Barrett’s esophagus.
12. What Role Does Diet Play In Managing Barrett’s Esophagus?
Diet plays a significant role in managing Barrett’s esophagus by reducing acid reflux and preventing irritation of the esophageal lining. Certain foods can trigger acid reflux, while others can help soothe the esophagus.
Key dietary considerations include:
- Foods to Avoid: Fatty foods, spicy foods, chocolate, caffeine, alcohol, and acidic fruits.
- Foods to Include: High-fiber foods, lean proteins, and non-acidic fruits and vegetables.
- Smaller Meals: Eating smaller, more frequent meals can reduce acid production.
- Hydration: Drinking plenty of water can help neutralize stomach acid.
Registered dietitians often recommend a tailored dietary plan to help manage GERD and Barrett’s esophagus symptoms.
13. How Does Barrett’s Esophagus Affect Quality Of Life?
Barrett’s esophagus can significantly impact quality of life, especially if symptoms are not well-managed. Chronic heartburn, regurgitation, and difficulty swallowing can interfere with daily activities and overall well-being.
Potential impacts on quality of life include:
- Physical Discomfort: Persistent heartburn and chest pain.
- Dietary Restrictions: Avoiding certain foods can limit dietary choices.
- Sleep Disturbances: Nighttime acid reflux can disrupt sleep.
- Anxiety: Concerns about developing esophageal cancer can cause anxiety.
Effective management of symptoms and regular surveillance can help improve quality of life for individuals with Barrett’s esophagus.
14. Is Barrett’s Esophagus More Common In Certain Populations?
Yes, Barrett’s esophagus is more common in certain populations. Several factors can increase the risk of developing this condition.
Populations at higher risk include:
- Men: Men are more likely to develop Barrett’s esophagus than women.
- Caucasians: Caucasians have a higher risk compared to other ethnic groups.
- Older Adults: The condition is more common in adults over the age of 50.
- Obese Individuals: Obesity increases the risk of GERD and Barrett’s esophagus.
- Smokers: Smoking is a known risk factor for GERD and esophageal damage.
Understanding these risk factors can help in identifying individuals who may benefit from screening and preventive measures.
15. What Are The Potential Complications Of Untreated Barrett’s Esophagus?
If left untreated, Barrett’s esophagus can lead to several complications, with the most concerning being the development of esophageal adenocarcinoma.
Other potential complications include:
- Esophageal Stricture: Narrowing of the esophagus due to inflammation and scarring.
- Esophageal Ulcer: Open sores in the esophageal lining.
- Bleeding: Chronic inflammation can lead to bleeding in the esophagus.
- Increased Cancer Risk: The risk of developing esophageal cancer increases significantly.
Regular surveillance and appropriate treatment are crucial in preventing these complications.
16. How Does Radiofrequency Ablation (RFA) Treat Barrett’s Esophagus?
Radiofrequency ablation (RFA) is a common endoscopic technique used to treat Barrett’s esophagus, particularly when dysplasia is present. RFA uses radiofrequency energy to destroy abnormal cells in the esophageal lining.
Key aspects of RFA include:
- Procedure: A catheter is inserted into the esophagus through an endoscope.
- Energy Delivery: Radiofrequency energy is delivered to the abnormal tissue.
- Cell Destruction: The energy heats and destroys the abnormal cells.
- Healing: The treated area heals, allowing normal esophageal lining to regrow.
According to research in Gastrointestinal Endoscopy, RFA is highly effective in eradicating dysplasia and reducing the risk of progression to esophageal cancer.
17. What Should I Expect During A Barrett’s Esophagus Endoscopy?
An endoscopy for Barrett’s esophagus involves inserting a thin, flexible tube with a camera into your esophagus to examine the lining. The procedure is typically performed by a gastroenterologist and usually takes about 15-30 minutes.
Here’s what to expect:
- Preparation: You’ll need to fast for several hours before the procedure.
- Sedation: You’ll receive medication to help you relax and stay comfortable.
- Procedure: The endoscope is gently guided through your mouth and into your esophagus.
- Examination: The doctor examines the lining of your esophagus for any abnormalities.
- Biopsy: If abnormalities are found, a small tissue sample (biopsy) may be taken for further examination.
- Recovery: You’ll be monitored for a short period after the procedure before being discharged.
Following the procedure, your doctor will discuss the results with you and recommend any necessary treatment or follow-up.
18. Can Children Develop Barrett’s Esophagus?
While Barrett’s esophagus is more commonly diagnosed in adults, children can also develop the condition, though it is rare. Risk factors and causes in children are similar to those in adults, primarily chronic acid reflux.
Important considerations for children include:
- Underlying Conditions: GERD in children may be associated with underlying conditions such as cerebral palsy or other neurological disorders.
- Diagnosis: Diagnosis involves endoscopy with biopsy, as in adults.
- Treatment: Treatment focuses on managing acid reflux with medications and lifestyle changes.
Pediatric gastroenterologists are best equipped to diagnose and manage Barrett’s esophagus in children.
19. What Is The Role Of The Lower Esophageal Sphincter (LES) In Barrett’s Esophagus?
The lower esophageal sphincter (LES) plays a crucial role in the development of Barrett’s esophagus. The LES is a muscular ring that acts as a valve between the esophagus and the stomach. Its primary function is to prevent stomach acid from flowing back into the esophagus.
In individuals with GERD, the LES may be weakened or malfunctioning, allowing stomach acid to frequently reflux into the esophagus. This chronic acid exposure can damage the esophageal lining and lead to the development of Barrett’s esophagus.
Maintaining the proper function of the LES is essential in preventing and managing GERD and Barrett’s esophagus.
20. How Is Barrett’s Esophagus Different From A Hiatal Hernia?
While Barrett’s esophagus and hiatal hernia are related to GERD, they are distinct conditions. A hiatal hernia occurs when the upper part of the stomach bulges through the diaphragm (the muscle that separates the chest and abdomen) and into the chest cavity.
Key differences include:
- Definition: Barrett’s esophagus involves changes in the esophageal lining, while a hiatal hernia is a structural abnormality.
- Cause: Both are associated with GERD, but a hiatal hernia can contribute to GERD by weakening the LES.
- Complications: Barrett’s esophagus increases the risk of esophageal cancer, while a hiatal hernia can cause heartburn, regurgitation, and chest pain.
Many individuals with Barrett’s esophagus also have a hiatal hernia, but the conditions require separate diagnosis and management.
21. What Are The Benefits Of Early Detection Of Barrett’s Esophagus?
Early detection of Barrett’s esophagus offers significant benefits in terms of managing the condition and preventing complications.
Key benefits include:
- Prevention of Cancer: Early detection allows for surveillance and treatment of dysplasia, preventing the progression to esophageal cancer.
- Improved Treatment Outcomes: Treatment is more effective when initiated at an early stage.
- Reduced Symptoms: Early management can alleviate symptoms such as heartburn and regurgitation.
- Enhanced Quality of Life: Timely intervention can improve overall quality of life by reducing physical discomfort and anxiety.
Regular screening is recommended for individuals at high risk of developing Barrett’s esophagus.
22. What Support Groups Are Available For People With Barrett’s Esophagus?
Support groups can be a valuable resource for individuals with Barrett’s esophagus, providing emotional support, education, and practical advice.
Potential resources include:
- Online Forums: Many online forums and communities offer support and information for individuals with Barrett’s esophagus.
- Patient Advocacy Groups: Organizations such as the American Cancer Society and the Esophageal Cancer Awareness Association provide resources and support for patients.
- Local Support Groups: Some hospitals and medical centers offer local support groups for individuals with digestive disorders.
Participating in support groups can help individuals cope with the challenges of living with Barrett’s esophagus and connect with others who share similar experiences.
23. Can Stress And Anxiety Worsen Barrett’s Esophagus Symptoms?
Yes, stress and anxiety can exacerbate symptoms of Barrett’s esophagus, primarily by increasing acid production and altering digestive function.
The impact of stress and anxiety includes:
- Increased Acid Production: Stress can stimulate the production of stomach acid, leading to more frequent reflux.
- Muscle Tension: Anxiety can cause muscle tension, which can worsen esophageal discomfort.
- Altered Eating Habits: Stress may lead to unhealthy eating habits, such as overeating or consuming trigger foods.
Managing stress through relaxation techniques, exercise, and counseling can help alleviate Barrett’s esophagus symptoms.
24. What Is The Long-Term Outlook For People With Barrett’s Esophagus?
The long-term outlook for individuals with Barrett’s esophagus depends on several factors, including the presence of dysplasia, the effectiveness of treatment, and adherence to surveillance recommendations.
General considerations include:
- Surveillance: Regular surveillance is essential to detect and manage any precancerous changes.
- Treatment Success: Successful treatment of dysplasia can significantly reduce the risk of esophageal cancer.
- Lifestyle Modifications: Adhering to lifestyle modifications can help manage symptoms and prevent complications.
With proper management and surveillance, most individuals with Barrett’s esophagus can maintain a good quality of life and prevent the development of esophageal cancer.
25. What Questions Should I Ask My Doctor About Barrett’s Esophagus?
When diagnosed with Barrett’s esophagus, it’s important to have a thorough discussion with your doctor to understand your condition and treatment options.
Key questions to ask include:
- What is the severity of my condition?
- Do I have dysplasia? If so, what grade?
- What treatment options are available to me?
- How often should I undergo surveillance?
- What lifestyle changes should I make?
- What are the potential risks and benefits of each treatment option?
- What is the likelihood of developing esophageal cancer?
- What support resources are available to me?
Having a clear understanding of your condition and treatment plan can help you make informed decisions and take proactive steps to manage your health.
26. How Can I Prevent Barrett’s Esophagus If I Have GERD?
If you have GERD, there are several steps you can take to reduce your risk of developing Barrett’s esophagus.
Preventive measures include:
- Manage GERD: Effectively manage GERD with medications and lifestyle changes.
- Follow Medical Advice: Adhere to your doctor’s recommendations for GERD management.
- Weight Management: Maintain a healthy weight to reduce abdominal pressure.
- Avoid Triggers: Avoid foods and beverages that trigger acid reflux.
- Elevate Head of Bed: Raise the head of your bed to prevent nighttime acid reflux.
- Quit Smoking: Smoking can worsen GERD and increase the risk of Barrett’s esophagus.
Taking these steps can significantly reduce your risk and improve your overall esophageal health.
27. Are There Any Alternative Therapies For Managing Barrett’s Esophagus?
While conventional medical treatments are the primary approach for managing Barrett’s esophagus, some individuals explore alternative therapies to complement their treatment plan.
Alternative therapies include:
- Acupuncture: May help reduce stress and improve digestive function.
- Herbal Remedies: Some herbs, such as ginger and chamomile, may help soothe the digestive system.
- Probiotics: May help improve gut health and reduce inflammation.
It’s important to discuss any alternative therapies with your doctor before starting them, as they may interact with conventional treatments or have potential side effects.
28. How Is The Success Of Barrett’s Esophagus Treatment Measured?
The success of Barrett’s esophagus treatment is typically measured by the eradication of dysplasia and the prevention of progression to esophageal cancer.
Key indicators of treatment success include:
- Eradication of Dysplasia: Absence of dysplasia on follow-up biopsies.
- Regression of Barrett’s Esophagus: Reduction in the length of the Barrett’s esophagus segment.
- Prevention of Cancer: No development of esophageal cancer during long-term surveillance.
- Symptom Relief: Alleviation of GERD symptoms and improved quality of life.
Regular follow-up and surveillance are essential to monitor treatment success and detect any recurrence of dysplasia.
29. What Research Is Currently Being Conducted On Barrett’s Esophagus?
Research on Barrett’s esophagus is ongoing, with a focus on improving detection, treatment, and prevention strategies.
Current research areas include:
- Biomarkers: Identifying biomarkers for early detection of dysplasia and cancer risk.
- Imaging Techniques: Developing advanced imaging techniques for improved surveillance.
- Therapeutic Interventions: Investigating new therapeutic interventions for treating dysplasia and preventing cancer.
- Genetic Factors: Understanding the genetic factors that contribute to the development of Barrett’s esophagus.
Staying informed about the latest research can help individuals make informed decisions about their care and participate in clinical trials if appropriate.
30. Where Can I Find More Information About Barrett’s Esophagus?
Numerous reliable resources provide comprehensive information about Barrett’s esophagus.
Recommended resources include:
- Mayo Clinic: Offers detailed information on symptoms, causes, diagnosis, and treatment.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Provides research-based information on digestive diseases.
- American Gastroenterological Association (AGA): Offers guidelines and resources for healthcare professionals and patients.
- American Cancer Society: Provides information on esophageal cancer and related conditions.
- Esophageal Cancer Awareness Association: Offers support and resources for individuals affected by esophageal cancer.
Consulting these resources can help you stay informed and make informed decisions about your health.
Experiencing persistent heartburn or acid reflux? Unsure about your digestive health? Don’t wait! Visit WHAT.EDU.VN today and ask our experts for free personalized advice. Our team is ready to answer all your questions and provide you with the information you need to take control of your health. Contact us at 888 Question City Plaza, Seattle, WA 98101, United States, Whatsapp: +1 (206) 555-7890, or visit our website at what.edu.vn. Your health questions answered, free of charge!