Cardiac function is vital, and understanding what it encompasses is essential for overall well-being. Are you looking for clear, concise answers about cardiac health? At WHAT.EDU.VN, we provide easily accessible information to empower you to take control of your cardiovascular health. We offer insights into maintaining a healthy heart rhythm and understanding potential heart valve problems. Let’s delve into cardiac anatomy, heart disease prevention, and heart failure management.
1. What Is Cardiac and What Does It Encompass?
Cardiac pertains to the heart. Understanding the term involves exploring the heart’s anatomy, function, and related conditions.
The term “cardiac” refers to anything related to the heart. This encompasses a wide range of aspects, including the heart’s structure, function, and any diseases or conditions that affect it. Understanding what cardiac encompasses is fundamental to comprehending cardiovascular health.
1.1. Exploring the Anatomy of the Heart
The heart is a complex organ, and knowing its parts is crucial for understanding cardiac function.
The heart comprises four chambers: the right atrium, right ventricle, left atrium, and left ventricle. These chambers work together to pump blood throughout the body. Valves, such as the mitral, tricuspid, aortic, and pulmonary valves, ensure that blood flows in the correct direction.
1.2. Understanding the Function of the Heart
The heart’s primary function is to circulate blood, delivering oxygen and nutrients to the body’s tissues.
The heart acts as a pump, contracting and relaxing to propel blood through the circulatory system. This process involves both electrical and mechanical activity. The sinoatrial (SA) node generates electrical impulses that regulate the heart rate.
1.3. Cardiac Conditions and Diseases
Cardiac conditions can range from congenital heart defects to acquired diseases like coronary artery disease.
Common cardiac conditions include:
- Coronary Artery Disease (CAD): Characterized by plaque buildup in the arteries, leading to reduced blood flow.
- Heart Failure: A condition in which the heart cannot pump enough blood to meet the body’s needs.
- Arrhythmias: Irregular heart rhythms, including both bradycardia (slow heart rate) and tachycardia (fast heart rate).
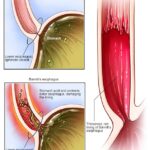
- Valve Disorders: Problems with the heart valves, such as stenosis (narrowing) or regurgitation (leaking).
- Cardiomyopathy: Diseases of the heart muscle.
- Congenital Heart Defects: Heart abnormalities present at birth.
1.4. Risk Factors for Cardiac Disease
Several factors can increase the risk of developing cardiac disease, including lifestyle choices and genetics.
Key risk factors include:
- High Blood Pressure: Damages arteries and increases the risk of heart disease and stroke.
- High Cholesterol: Leads to plaque buildup in arteries.
- Smoking: Damages blood vessels and increases the risk of blood clots.
- Diabetes: Increases the risk of heart disease and stroke.
- Obesity: Contributes to high blood pressure, high cholesterol, and diabetes.
- Family History: Genetic predisposition to heart disease.
- Poor Diet: High in saturated fats, trans fats, and sodium.
- Physical Inactivity: Lack of exercise increases the risk of heart disease.
- Age: The risk of heart disease increases with age.
- Stress: Chronic stress can damage the heart and blood vessels.
1.5. Diagnostic Tests for Cardiac Health
Various diagnostic tests can help assess cardiac function and detect potential problems.
Common tests include:
- Electrocardiogram (ECG or EKG): Records the electrical activity of the heart.
- Echocardiogram: Uses ultrasound to create images of the heart.
- Stress Test: Monitors heart function during exercise.
- Cardiac Catheterization: Involves inserting a catheter into a blood vessel to examine the heart.
- CT Scan and MRI: Provide detailed images of the heart and blood vessels.
- Blood Tests: Measure cholesterol levels, blood sugar, and other markers of heart health.
1.6. Maintaining Cardiac Health
Adopting a heart-healthy lifestyle can significantly reduce the risk of cardiac disease.
Key strategies for maintaining cardiac health include:
- Healthy Diet: Emphasize fruits, vegetables, whole grains, and lean protein.
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity exercise per week.
- Quit Smoking: Smoking cessation is crucial for heart health.
- Manage Blood Pressure: Keep blood pressure within healthy ranges.
- Control Cholesterol: Lower LDL (bad) cholesterol and raise HDL (good) cholesterol.
- Maintain a Healthy Weight: Achieve and maintain a healthy body weight.
- Manage Stress: Practice stress-reduction techniques such as yoga and meditation.
- Regular Check-ups: Schedule regular check-ups with your healthcare provider.
1.7. Common Treatments for Cardiac Conditions
Treatments for cardiac conditions vary depending on the specific condition and its severity.
Common treatments include:
- Medications: Such as ACE inhibitors, beta-blockers, statins, and antiarrhythmics.
- Lifestyle Changes: Including diet, exercise, and smoking cessation.
- Angioplasty and Stenting: Procedures to open blocked arteries.
- Bypass Surgery: Creating new pathways for blood to flow around blocked arteries.
- Pacemaker Implantation: For treating slow heart rates.
- Defibrillator Implantation: For preventing sudden cardiac arrest.
- Valve Repair or Replacement: For treating valve disorders.
1.8. The Role of Cardiac Rehabilitation
Cardiac rehabilitation programs can help individuals recover from heart events and improve their overall heart health.
Cardiac rehabilitation typically involves:
- Exercise Training: Supervised exercise sessions to improve cardiovascular fitness.
- Education: Information on heart-healthy living, including diet, exercise, and medication management.
- Counseling: Support for managing stress, anxiety, and depression.
1.9. Recent Advances in Cardiac Care
Advances in technology and medical research continue to improve cardiac care.
Recent advances include:
- Transcatheter Valve Replacement: Minimally invasive procedures to replace heart valves.
- Left Atrial Appendage Closure: A procedure to reduce the risk of stroke in individuals with atrial fibrillation.
- Advanced Imaging Techniques: Such as 3D echocardiography and cardiac MRI.
- New Medications: Such as novel anticoagulants and cholesterol-lowering drugs.
1.10. The Impact of Genetics on Cardiac Health
Genetics can play a significant role in the development of cardiac disease.
Understanding your family history can help you assess your risk and take preventive measures. Genetic testing may be recommended in certain cases.
Cardiac health is a multifaceted topic encompassing the heart’s anatomy, function, and related conditions. By understanding the risk factors, diagnostic tests, and treatment options, individuals can take proactive steps to maintain and improve their cardiovascular well-being. At WHAT.EDU.VN, we aim to provide comprehensive and accessible information to empower you in your journey toward a healthier heart. Contact us at 888 Question City Plaza, Seattle, WA 98101, United States, or WhatsApp us at +1 (206) 555-7890 for more information.
2. How Does Cardiac Relate to Cardiovascular Health?
Cardiac is a key component of cardiovascular health, impacting circulation and overall well-being.
The term “cardiac” is intrinsically linked to cardiovascular health, referring specifically to the heart’s role within the broader cardiovascular system. The cardiovascular system encompasses the heart and blood vessels, working together to circulate blood throughout the body, delivering oxygen and nutrients to cells and removing waste products. Understanding the relationship between cardiac function and cardiovascular health is essential for maintaining overall well-being.
2.1. The Cardiovascular System Explained
The cardiovascular system’s main components are the heart, blood vessels (arteries, veins, and capillaries), and blood.
- Heart: The central pump that drives blood circulation.
- Arteries: Vessels that carry oxygenated blood away from the heart.
- Veins: Vessels that return deoxygenated blood to the heart.
- Capillaries: Tiny blood vessels that facilitate the exchange of oxygen, nutrients, and waste products between the blood and tissues.
- Blood: The fluid that carries oxygen, nutrients, hormones, and waste products throughout the body.
2.2. Cardiac Function and Blood Circulation
Effective cardiac function is essential for maintaining proper blood circulation throughout the body.
The heart’s pumping action ensures that blood is continuously circulated through the arteries, capillaries, and veins. This circulation delivers oxygen and nutrients to the body’s tissues and removes waste products.
2.3. The Impact of Cardiac Health on Other Organs
Cardiac health directly affects the function of other organs in the body.
When the heart functions efficiently, organs receive the oxygen and nutrients they need to operate properly. Conversely, when the heart is compromised, it can lead to organ dysfunction and systemic health issues.
2.4. Cardiac Output and Its Significance
Cardiac output, the amount of blood the heart pumps per minute, is a critical measure of cardiac function.
Cardiac output is determined by heart rate (the number of beats per minute) and stroke volume (the amount of blood pumped with each beat). Maintaining adequate cardiac output is essential for meeting the body’s metabolic demands.
2.5. Common Cardiac Conditions Affecting Cardiovascular Health
Various cardiac conditions can impact cardiovascular health, including coronary artery disease, heart failure, and arrhythmias.
- Coronary Artery Disease (CAD): Reduces blood flow to the heart muscle, leading to chest pain (angina) and heart attack.
- Heart Failure: Impairs the heart’s ability to pump blood effectively, leading to fluid buildup and shortness of breath.
- Arrhythmias: Irregular heart rhythms can disrupt blood flow and cause palpitations, dizziness, or fainting.
- Valve Disorders: Such as stenosis or regurgitation, can strain the heart and lead to heart failure.
- Cardiomyopathy: Diseases of the heart muscle can impair its ability to contract and relax properly.
- Congenital Heart Defects: Can affect the heart’s structure and function, leading to various cardiovascular problems.
2.6. The Role of Blood Vessels in Cardiovascular Health
Healthy blood vessels are essential for maintaining optimal cardiovascular function.
Arteries should be flexible and free of plaque buildup to ensure smooth blood flow. Veins should effectively return blood to the heart, preventing blood clots and other complications.
2.7. Maintaining Healthy Blood Pressure
Blood pressure is a measure of the force of blood against the artery walls.
Maintaining healthy blood pressure levels is crucial for cardiovascular health. High blood pressure (hypertension) can damage blood vessels and increase the risk of heart disease, stroke, and kidney disease.
2.8. The Importance of Cholesterol Management
Cholesterol is a fatty substance found in the blood.
Managing cholesterol levels is essential for preventing plaque buildup in arteries. High levels of LDL (bad) cholesterol increase the risk of atherosclerosis, while high levels of HDL (good) cholesterol help protect against heart disease.
2.9. Lifestyle Factors Influencing Cardiovascular Health
Lifestyle factors play a significant role in determining cardiovascular health.
- Healthy Diet: A diet rich in fruits, vegetables, whole grains, and lean protein can help lower blood pressure, cholesterol, and the risk of heart disease.
- Regular Exercise: Physical activity can improve cardiovascular fitness, lower blood pressure, and help maintain a healthy weight.
- Smoking Cessation: Smoking damages blood vessels and increases the risk of heart disease and stroke.
- Stress Management: Chronic stress can damage the heart and blood vessels.
- Moderate Alcohol Consumption: Excessive alcohol consumption can raise blood pressure and increase the risk of heart disease.
2.10. Medical Treatments for Cardiovascular Conditions
Various medical treatments are available for managing cardiovascular conditions.
- Medications: Such as ACE inhibitors, beta-blockers, statins, and antiplatelet drugs.
- Angioplasty and Stenting: Procedures to open blocked arteries.
- Bypass Surgery: Creating new pathways for blood to flow around blocked arteries.
- Pacemaker Implantation: For treating slow heart rates.
- Defibrillator Implantation: For preventing sudden cardiac arrest.
- Valve Repair or Replacement: For treating valve disorders.
Understanding the relationship between cardiac function and cardiovascular health is crucial for preventing and managing heart disease. By adopting a heart-healthy lifestyle and seeking appropriate medical care, individuals can significantly reduce their risk of cardiovascular problems. At WHAT.EDU.VN, we offer comprehensive information and resources to help you maintain optimal cardiovascular health. Contact us at 888 Question City Plaza, Seattle, WA 98101, United States, or WhatsApp us at +1 (206) 555-7890 for personalized guidance.
3. What Is Cardiac Arrest and How Does It Differ from a Heart Attack?
Cardiac arrest and heart attack are distinct but related conditions, each with different mechanisms and treatments.
Cardiac arrest and heart attack are two distinct yet often confused medical emergencies involving the heart. Understanding the differences between them is crucial for recognizing symptoms and seeking appropriate medical attention.
3.1. Defining Cardiac Arrest
Cardiac arrest is the sudden cessation of heart function, leading to loss of consciousness and breathing.
Cardiac arrest occurs when the heart’s electrical system malfunctions, causing the heart to stop beating effectively. This results in a sudden loss of blood flow to the brain and other vital organs.
3.2. Defining Heart Attack
A heart attack, also known as myocardial infarction, occurs when blood flow to a part of the heart is blocked.
A heart attack typically occurs when a blood clot forms in a coronary artery, blocking the flow of blood to the heart muscle. This can damage or kill part of the heart muscle.
3.3. Key Differences Between Cardiac Arrest and Heart Attack
The primary difference lies in the underlying mechanism and immediate consequences.
| Feature | Cardiac Arrest | Heart Attack |
|---|---|---|
| Mechanism | Sudden electrical malfunction causing the heart to stop beating effectively | Blockage of blood flow to a part of the heart muscle, usually by a blood clot |
| Consequences | Immediate loss of consciousness, no pulse, no breathing | Chest pain, shortness of breath, nausea, and other symptoms |
| Immediate Action | CPR and defibrillation | Medical treatment to restore blood flow to the heart |
3.4. Causes of Cardiac Arrest
Several factors can trigger cardiac arrest, including heart conditions, electrical abnormalities, and trauma.
Common causes include:
- Ventricular Fibrillation: A life-threatening arrhythmia in which the heart’s ventricles quiver instead of pumping effectively.
- Coronary Artery Disease: Can lead to sudden blockage of blood flow to the heart.
- Cardiomyopathy: Diseases of the heart muscle can increase the risk of arrhythmias and cardiac arrest.
- Electrolyte Imbalances: Such as low potassium or magnesium levels.
- Drug Overdose: Certain drugs can trigger arrhythmias and cardiac arrest.
- Trauma: Severe injuries can lead to cardiac arrest.
3.5. Causes of Heart Attack
Heart attacks are typically caused by coronary artery disease, leading to a sudden blockage.
The most common cause of heart attack is:
- Coronary Artery Disease (CAD): Plaque buildup in the arteries can rupture, leading to the formation of a blood clot that blocks blood flow to the heart.
3.6. Recognizing the Symptoms of Cardiac Arrest
The signs of cardiac arrest are immediate and unmistakable.
Symptoms include:
- Sudden Loss of Consciousness: The person collapses and becomes unresponsive.
- No Pulse: The person’s heart has stopped beating effectively.
- No Breathing: The person is not breathing or is only gasping for air.
3.7. Recognizing the Symptoms of Heart Attack
Heart attack symptoms can vary but often include chest pain and discomfort.
Common symptoms include:
- Chest Pain or Discomfort: A feeling of pressure, squeezing, or fullness in the chest.
- Shortness of Breath: Difficulty breathing or feeling breathless.
- Pain or Discomfort in Other Areas: Such as the arms, shoulder, neck, jaw, or back.
- Nausea or Vomiting: Feeling sick to your stomach.
- Lightheadedness or Dizziness: Feeling faint or unsteady.
- Sweating: Breaking out in a cold sweat.
3.8. Immediate Actions for Cardiac Arrest
Immediate action is critical for improving the chances of survival.
- Call Emergency Services: Dial the local emergency number immediately.
- Start CPR: Perform chest compressions and rescue breaths if trained.
- Use an AED (Automated External Defibrillator): If available, follow the device’s instructions.
3.9. Immediate Actions for Heart Attack
Prompt medical attention can minimize damage to the heart muscle.
- Call Emergency Services: Dial the local emergency number immediately.
- Chew Aspirin: If recommended by a healthcare professional, chew an aspirin to help prevent further blood clotting.
- Stay Calm: Try to remain calm while waiting for medical assistance.
3.10. Long-Term Management and Prevention
Both cardiac arrest and heart attack require long-term management to prevent future events.
For cardiac arrest survivors:
- Implantable Cardioverter-Defibrillator (ICD): A device that can detect and correct life-threatening arrhythmias.
- Medications: To manage underlying heart conditions and prevent arrhythmias.
- Lifestyle Changes: Including diet, exercise, and smoking cessation.
For heart attack survivors:
- Medications: Such as beta-blockers, ACE inhibitors, statins, and antiplatelet drugs.
- Cardiac Rehabilitation: A program to help improve cardiovascular fitness and manage risk factors.
- Lifestyle Changes: Including diet, exercise, and smoking cessation.
Understanding the differences between cardiac arrest and heart attack is essential for recognizing symptoms and seeking appropriate medical attention. Immediate action, including CPR and calling emergency services, can significantly improve the chances of survival. At WHAT.EDU.VN, we provide comprehensive information and resources to help you understand and manage cardiac conditions. Contact us at 888 Question City Plaza, Seattle, WA 98101, United States, or WhatsApp us at +1 (206) 555-7890 for expert guidance.
4. What Is Cardiac Ablation and When Is It Necessary?
Cardiac ablation is a procedure used to correct heart rhythm problems, improving quality of life.
Cardiac ablation is a medical procedure used to correct heart rhythm problems (arrhythmias). It involves destroying small areas of heart tissue that are causing the abnormal heartbeats. Understanding when cardiac ablation is necessary and how it works can help individuals make informed decisions about their treatment options.
4.1. Understanding Arrhythmias
Arrhythmias are irregular heart rhythms that can affect the heart’s ability to pump blood effectively.
Arrhythmias can cause the heart to beat too fast (tachycardia), too slow (bradycardia), or irregularly. Common types of arrhythmias include atrial fibrillation, atrial flutter, supraventricular tachycardia (SVT), and ventricular tachycardia.
4.2. The Purpose of Cardiac Ablation
Cardiac ablation aims to restore a normal heart rhythm by eliminating the source of the arrhythmia.
The procedure involves identifying the specific area of heart tissue that is causing the abnormal heartbeats and then using energy to destroy or isolate that tissue.
4.3. Types of Cardiac Ablation
Different techniques can be used for cardiac ablation, depending on the type and location of the arrhythmia.
Common types of cardiac ablation include:
- Radiofrequency Ablation: Uses heat energy to destroy the problematic heart tissue.
- Cryoablation: Uses cold energy to freeze and destroy the tissue.
- Surgical Ablation: Involves open-heart surgery to access and ablate the tissue.
4.4. When Is Cardiac Ablation Necessary?
Cardiac ablation is typically recommended when arrhythmias are causing significant symptoms or when medications are not effective.
Indications for cardiac ablation include:
- Atrial Fibrillation: When medications cannot control the heart rate or rhythm.
- Atrial Flutter: Often treated with ablation due to its high success rate.
- Supraventricular Tachycardia (SVT): When medications are not effective or cause significant side effects.
- Ventricular Tachycardia: To prevent life-threatening arrhythmias in individuals with heart disease.
4.5. The Cardiac Ablation Procedure
The procedure typically involves inserting catheters into blood vessels and guiding them to the heart.
During the procedure:
- Catheter Insertion: A catheter is inserted into a blood vessel, usually in the groin or arm, and guided to the heart.
- Electrophysiological Mapping: The catheter is used to map the electrical activity of the heart and identify the source of the arrhythmia.
- Ablation: Energy is delivered through the catheter to destroy or isolate the problematic heart tissue.
- Post-Ablation Monitoring: The heart is monitored to ensure the arrhythmia has been eliminated.
4.6. Risks and Complications of Cardiac Ablation
Like any medical procedure, cardiac ablation carries potential risks and complications.
Possible risks include:
- Bleeding or Infection: At the catheter insertion site.
- Blood Vessel Damage: From catheter insertion.
- Pericardial Effusion: Fluid buildup around the heart.
- Pulmonary Vein Stenosis: Narrowing of the pulmonary veins.
- Heart Block: Damage to the heart’s electrical system, requiring a pacemaker.
- Stroke: Due to blood clots forming during the procedure.
4.7. Success Rates of Cardiac Ablation
Success rates vary depending on the type of arrhythmia and the individual’s overall health.
Ablation is often highly effective for treating arrhythmias such as SVT and atrial flutter. Success rates for atrial fibrillation ablation can vary, with some individuals requiring multiple procedures.
4.8. Recovery After Cardiac Ablation
Recovery typically involves a short hospital stay and some restrictions on activity.
After the procedure:
- Hospital Stay: Usually one to two days.
- Activity Restrictions: Avoid strenuous activities for a few weeks.
- Medications: May be prescribed to prevent blood clots or control heart rate.
- Follow-Up Appointments: To monitor heart rhythm and assess the success of the procedure.
4.9. Long-Term Management After Ablation
Long-term management may include medications and lifestyle changes to maintain a normal heart rhythm.
- Medications: Such as antiarrhythmics or blood thinners.
- Lifestyle Changes: Including diet, exercise, and stress management.
- Regular Check-Ups: To monitor heart rhythm and overall health.
4.10. Alternatives to Cardiac Ablation
Alternatives to cardiac ablation include medications and lifestyle changes to manage arrhythmias.
- Medications: Antiarrhythmic drugs can help control heart rate and rhythm.
- Lifestyle Changes: Including diet, exercise, and stress management.
- Watchful Waiting: In some cases, if symptoms are mild, monitoring the arrhythmia without intervention may be appropriate.
Cardiac ablation is a valuable treatment option for individuals with arrhythmias that are not well-controlled with medications. Understanding the procedure, its risks and benefits, and the recovery process can help individuals make informed decisions about their care. At WHAT.EDU.VN, we provide comprehensive information and resources to help you understand and manage cardiac conditions. Contact us at 888 Question City Plaza, Seattle, WA 98101, United States, or WhatsApp us at +1 (206) 555-7890 for personalized guidance.
5. What Is Cardiac Output and Why Is It Important?
Cardiac output is a key indicator of heart function, essential for delivering oxygen and nutrients throughout the body.
Cardiac output (CO) refers to the amount of blood the heart pumps per minute. It is a critical indicator of how well the heart is functioning and its ability to meet the body’s metabolic demands. Understanding what cardiac output is and why it is important can help individuals appreciate the significance of maintaining good cardiovascular health.
5.1. Defining Cardiac Output
Cardiac output is the volume of blood pumped by the heart each minute, measured in liters per minute (L/min).
Cardiac output is determined by two main factors:
- Heart Rate (HR): The number of times the heart beats per minute (beats/min).
- Stroke Volume (SV): The amount of blood pumped by the heart with each beat (mL/beat).
The formula for calculating cardiac output is:
CO = HR x SV
5.2. Normal Cardiac Output
Normal cardiac output typically ranges from 4 to 8 liters per minute in a healthy adult at rest.
Cardiac output can vary depending on factors such as age, body size, and activity level. During exercise, cardiac output can increase significantly to meet the body’s increased oxygen demands.
5.3. Factors Affecting Cardiac Output
Several factors can influence cardiac output, including heart rate, stroke volume, and the heart’s contractility.
Key factors affecting cardiac output include:
- Heart Rate: Increased heart rate can increase cardiac output, up to a certain point.
- Stroke Volume: Increased stroke volume can increase cardiac output.
- Contractility: The force with which the heart muscle contracts.
- Preload: The amount of blood filling the heart before it contracts.
- Afterload: The resistance the heart must overcome to pump blood out.
5.4. Why Cardiac Output Is Important
Cardiac output is essential for delivering oxygen and nutrients to the body’s tissues and removing waste products.
Adequate cardiac output is necessary for:
- Oxygen Delivery: Ensuring that all organs and tissues receive enough oxygen to function properly.
- Nutrient Delivery: Transporting nutrients to cells for energy production and growth.
- Waste Removal: Removing carbon dioxide and other waste products from the body.
- Maintaining Blood Pressure: Helping to regulate blood pressure and maintain adequate tissue perfusion.
5.5. Low Cardiac Output
Low cardiac output can result from various heart conditions and can lead to serious health problems.
Conditions that can cause low cardiac output include:
- Heart Failure: The heart cannot pump enough blood to meet the body’s needs.
- Cardiomyopathy: Diseases of the heart muscle can impair its ability to contract and relax properly.
- Valve Disorders: Such as stenosis or regurgitation, can strain the heart and reduce cardiac output.
- Arrhythmias: Irregular heart rhythms can disrupt blood flow and reduce cardiac output.
- Hypovolemia: Low blood volume due to dehydration or blood loss.
5.6. Symptoms of Low Cardiac Output
Symptoms of low cardiac output can vary depending on the severity and underlying cause.
Common symptoms include:
- Fatigue: Feeling tired and weak.
- Shortness of Breath: Difficulty breathing, especially during exercise.
- Dizziness or Lightheadedness: Feeling faint or unsteady.
- Confusion: Difficulty thinking clearly or remembering things.
- Cold and Clammy Skin: Due to reduced blood flow to the extremities.
- Swelling: In the legs, ankles, or abdomen due to fluid buildup.
5.7. Measuring Cardiac Output
Various methods can be used to measure cardiac output, both invasively and non-invasively.
Common methods include:
- Echocardiography: Uses ultrasound to estimate cardiac output.
- Cardiac Catheterization: Involves inserting a catheter into a blood vessel to measure cardiac output directly.
- Doppler Ultrasound: Measures blood flow velocity to estimate cardiac output.
- Impedance Cardiography: Measures electrical impedance to estimate cardiac output.
5.8. Improving Cardiac Output
Improving cardiac output involves addressing the underlying causes and optimizing heart function.
Strategies for improving cardiac output include:
- Medications: Such as ACE inhibitors, beta-blockers, and diuretics.
- Lifestyle Changes: Including diet, exercise, and smoking cessation.
- Fluid Management: Maintaining adequate hydration and managing fluid balance.
- Treating Underlying Conditions: Such as heart failure, valve disorders, or arrhythmias.
5.9. Cardiac Output During Exercise
Cardiac output increases significantly during exercise to meet the body’s increased oxygen demands.
During exercise:
- Heart Rate Increases: To pump more blood per minute.
- Stroke Volume Increases: To deliver more blood with each beat.
- Blood Flow Redistribution: More blood is directed to the working muscles.
5.10. Monitoring Cardiac Output in Critical Care
Monitoring cardiac output is essential in critical care settings to assess cardiovascular function and guide treatment.
Cardiac output monitoring can help healthcare providers:
- Assess Hemodynamic Status: Evaluate the patient’s circulatory function.
- Guide Fluid Management: Optimize fluid balance to maintain adequate cardiac output.
- Evaluate Response to Treatment: Assess the effectiveness of medications and other interventions.
Understanding cardiac output and its significance is crucial for maintaining good cardiovascular health. By monitoring cardiac output and addressing any underlying conditions, individuals can optimize heart function and improve their overall well-being. At WHAT.EDU.VN, we provide comprehensive information and resources to help you understand and manage cardiac conditions. Contact us at 888 Question City Plaza, Seattle, WA 98101, United States, or WhatsApp us at +1 (206) 555-7890 for personalized guidance.
Don’t struggle with unanswered questions. Visit what.edu.vn today and get the free answers you need!