Myeloma disease explained simply. Are you looking for clear answers about myeloma disease? WHAT.EDU.VN provides reliable information on this condition, from its causes and symptoms to diagnosis and treatment options. Get free answers and explore related topics like plasma cell myeloma and multiple myeloma.
1. What Is Myeloma Disease?
Myeloma disease, also known as multiple myeloma, is a type of cancer that affects plasma cells. These are white blood cells responsible for producing antibodies to fight infection. In myeloma, abnormal plasma cells accumulate in the bone marrow, disrupting the production of normal blood cells and causing various health problems. According to a study by the American Cancer Society, multiple myeloma accounts for about 1% of all cancers.
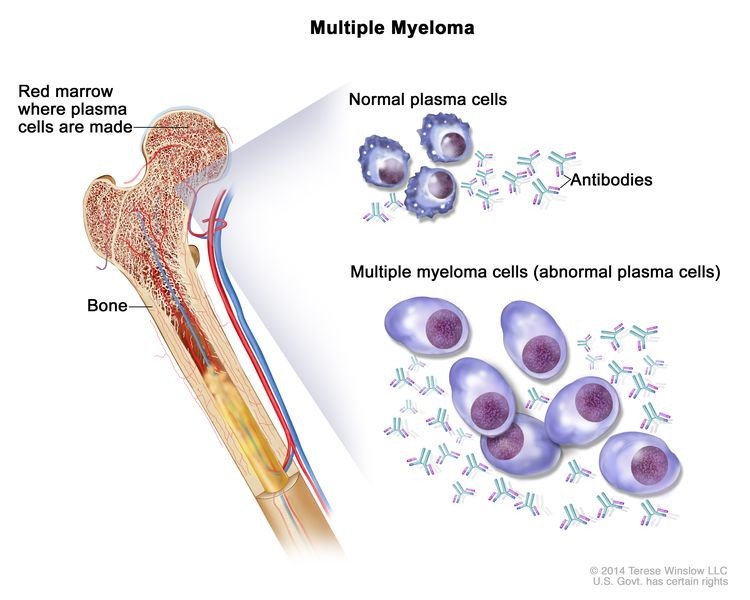 Multiple myeloma cells building up in bone marrow
Multiple myeloma cells building up in bone marrow
2. What Are the Different Types of Myeloma?
Myeloma encompasses several types, each with unique characteristics and prognoses:
2.1. Multiple Myeloma
Multiple myeloma is the most common type, characterized by the accumulation of abnormal plasma cells in the bone marrow, leading to tumors in multiple bones. This can result in bone pain, fractures, and other complications. As stated by the International Myeloma Foundation, early diagnosis and treatment are crucial for managing multiple myeloma effectively.
2.2. Smoldering Multiple Myeloma (SMM)
Smoldering multiple myeloma is a precursor to active multiple myeloma. It is defined by the presence of abnormal plasma cells in the bone marrow and M protein in the blood or urine. However, individuals with SMM do not exhibit the typical symptoms or organ damage associated with active myeloma. According to research published in the journal “Blood,” close monitoring of patients with SMM is essential to detect progression to active myeloma.
2.3. Solitary Plasmacytoma
Solitary plasmacytoma involves a single tumor of abnormal plasma cells, typically found in bone or soft tissue. Unlike multiple myeloma, solitary plasmacytomas do not involve widespread bone marrow involvement. Treatment often involves radiation therapy or surgery to remove the tumor. A study in the “International Journal of Radiation Oncology, Biology, Physics” showed that radiation therapy is highly effective in controlling solitary plasmacytomas.
2.4. Extramedullary Plasmacytoma
Extramedullary plasmacytoma occurs when plasma cell tumors develop in tissues outside the bone marrow, such as the nasal passages, throat, or sinuses. These tumors are often treated with radiation therapy or surgery. The Mayo Clinic Proceedings published a study highlighting the importance of accurate diagnosis and timely treatment of extramedullary plasmacytomas.
2.5. Monoclonal Gammopathy of Undetermined Significance (MGUS)
MGUS is a condition in which abnormal plasma cells produce M protein, but there are no symptoms or signs of myeloma. It is considered a premalignant condition, as some individuals with MGUS may eventually develop multiple myeloma or other related disorders. Regular monitoring is recommended to detect any signs of progression. A report by the National Cancer Institute indicates that approximately 1% of individuals with MGUS develop multiple myeloma each year.
3. What Are the Signs and Symptoms of Myeloma?
Myeloma symptoms can vary widely, depending on the stage and severity of the disease:
3.1. Bone Pain
Bone pain, especially in the back, ribs, or hips, is a common symptom. The pain may be persistent and worsen with movement. The American Society of Clinical Oncology (ASCO) notes that bone pain is often the first symptom that patients notice.
3.2. Fractures
Myeloma can weaken bones, making them more prone to fractures. These fractures can occur even with minor injuries. The Myeloma Beacon emphasizes the importance of early diagnosis to prevent fractures and other skeletal complications.
3.3. Fatigue
Persistent fatigue and weakness are common due to the anemia caused by myeloma cells crowding out normal blood cells in the bone marrow. A study published in the journal “Leukemia & Lymphoma” found that fatigue significantly impacts the quality of life for myeloma patients.
3.4. Frequent Infections
Myeloma can suppress the immune system, increasing the risk of infections. Patients may experience recurrent colds, pneumonia, or other infections. The University of Arkansas for Medical Sciences reports that infections are a leading cause of morbidity and mortality in myeloma patients.
3.5. Kidney Problems
Myeloma proteins can damage the kidneys, leading to kidney dysfunction or failure. Symptoms may include swelling, shortness of breath, and decreased urine output. The National Kidney Foundation highlights the importance of monitoring kidney function in myeloma patients.
3.6. Hypercalcemia
Hypercalcemia, or high levels of calcium in the blood, can occur when myeloma cells break down bone. Symptoms may include nausea, constipation, confusion, and excessive thirst. The Cleveland Clinic notes that hypercalcemia can lead to serious complications if left untreated.
3.7. Anemia
Anemia, or a low red blood cell count, is common in myeloma patients due to the bone marrow being crowded with cancerous plasma cells. Symptoms may include fatigue, weakness, and shortness of breath. The Leukemia & Lymphoma Society emphasizes the need for effective anemia management in myeloma patients.
3.8. Neurological Symptoms
In some cases, myeloma can affect the nervous system, leading to symptoms such as numbness, tingling, or weakness in the arms or legs. The Peripheral Neuropathy Awareness Foundation provides resources for patients experiencing neurological complications of myeloma.
4. What Causes Myeloma Disease?
The exact cause of myeloma remains unclear, but several risk factors have been identified:
4.1. Genetic Factors
Genetic abnormalities, such as translocations and deletions in chromosomes, are commonly found in myeloma cells. These genetic changes can disrupt normal cell growth and lead to cancer. Research published in “Nature Reviews Cancer” suggests that genetic profiling can help predict prognosis and guide treatment decisions.
4.2. Age
The risk of myeloma increases with age, with most cases diagnosed in people over 65. The American Cancer Society reports that the median age at diagnosis is 69.
4.3. Race
Myeloma is more common in African Americans than in Caucasians. Studies at the Mayo Clinic have shown that African Americans are twice as likely to develop myeloma.
4.4. Family History
Having a family history of myeloma or other plasma cell disorders increases the risk. The Multiple Myeloma Research Foundation notes that while myeloma is not typically inherited, familial clustering can occur.
4.5. Exposure to Radiation or Chemicals
Exposure to high doses of radiation or certain chemicals, such as benzene, may increase the risk. The Centers for Disease Control and Prevention (CDC) provides information on occupational exposures and cancer risk.
4.6. Monoclonal Gammopathy of Undetermined Significance (MGUS)
MGUS, a premalignant condition, increases the risk of developing myeloma. Individuals with MGUS should be monitored regularly for signs of progression. The International Myeloma Working Group recommends risk stratification for MGUS patients to determine the frequency of monitoring.
5. How Is Myeloma Diagnosed?
Diagnosing myeloma involves a combination of tests and procedures:
5.1. Blood Tests
Blood tests can detect abnormal levels of M protein, calcium, and other markers associated with myeloma. The serum protein electrophoresis (SPEP) test is commonly used to identify M protein. The University of California, San Francisco (UCSF), explains the role of blood tests in myeloma diagnosis.
5.2. Urine Tests
Urine tests can detect Bence Jones protein, a type of M protein that is found in the urine of some myeloma patients. The 24-hour urine protein electrophoresis (UPEP) test is used to measure Bence Jones protein levels. The Binding Site provides resources on urine tests for myeloma diagnosis.
5.3. Bone Marrow Biopsy
A bone marrow biopsy involves removing a sample of bone marrow for examination under a microscope. This test can confirm the presence of myeloma cells and assess the extent of bone marrow involvement. The American Society for Clinical Pathology (ASCP) offers guidelines for bone marrow biopsy procedures.
5.4. Imaging Tests
Imaging tests, such as X-rays, MRI, and PET scans, can detect bone damage and tumors associated with myeloma. Whole-body low-dose CT scans are increasingly used for myeloma staging. The Radiological Society of North America (RSNA) provides information on imaging techniques for myeloma diagnosis.
5.5. Immunofixation
Immunofixation is a technique used to identify the specific type of M protein present in the blood or urine. This information can help guide treatment decisions. The Mayo Clinic Laboratories offers immunofixation testing for myeloma diagnosis.
5.6. Free Light Chain Assay
The free light chain assay measures the levels of kappa and lambda light chains in the blood. Abnormal ratios of these light chains can indicate the presence of myeloma. The National Comprehensive Cancer Network (NCCN) guidelines recommend the free light chain assay for myeloma diagnosis and monitoring.
6. What Are the Treatment Options for Myeloma?
Myeloma treatment aims to control the disease, relieve symptoms, and improve quality of life:
6.1. Chemotherapy
Chemotherapy involves using drugs to kill myeloma cells. It may be used as part of the initial treatment or to treat relapsed disease. The Dana-Farber Cancer Institute provides information on chemotherapy regimens for myeloma.
6.2. Targeted Therapy
Targeted therapy drugs specifically target myeloma cells while sparing normal cells. Examples include proteasome inhibitors (e.g., bortezomib, carfilzomib) and immunomodulatory drugs (e.g., lenalidomide, pomalidomide). Research published in the “New England Journal of Medicine” has demonstrated the efficacy of targeted therapy in myeloma treatment.
6.3. Immunotherapy
Immunotherapy uses the body’s immune system to fight myeloma cells. Examples include monoclonal antibodies (e.g., daratumumab, elotuzumab) and CAR T-cell therapy. The Fred Hutchinson Cancer Research Center is a leader in immunotherapy research for myeloma.
6.4. Stem Cell Transplantation
Stem cell transplantation involves replacing damaged bone marrow with healthy stem cells. It may be autologous (using the patient’s own stem cells) or allogeneic (using stem cells from a donor). The Blood & Marrow Transplantation Information Network (BMT InfoNet) provides resources for patients undergoing stem cell transplantation.
6.5. Radiation Therapy
Radiation therapy uses high-energy rays to kill myeloma cells and relieve bone pain. It may be used to treat solitary plasmacytomas or to manage localized bone pain in multiple myeloma. The American Society for Radiation Oncology (ASTRO) offers guidelines for radiation therapy in myeloma treatment.
6.6. Bisphosphonates
Bisphosphonates are drugs that help strengthen bones and prevent fractures in myeloma patients. They may be administered intravenously or orally. The Paget Foundation provides information on bisphosphonates and bone health.
6.7. Supportive Care
Supportive care includes treatments to manage symptoms and side effects of myeloma and its treatment. Examples include pain management, infection prevention, and nutritional support. The Multinational Association of Supportive Care in Cancer (MASCC) provides guidelines for supportive care in cancer patients.
7. What Is the Prognosis for Myeloma?
The prognosis for myeloma varies depending on several factors, including the stage of the disease, genetic abnormalities, and response to treatment. Advances in treatment have significantly improved survival rates in recent years.
7.1. Survival Rates
The five-year survival rate for myeloma is approximately 55%. However, survival rates vary depending on the stage of the disease at diagnosis. The National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program provides statistics on cancer survival rates.
7.2. Risk Stratification
Risk stratification involves assessing the risk of disease progression and tailoring treatment accordingly. The International Staging System (ISS) and Revised International Staging System (R-ISS) are commonly used for risk stratification in myeloma. The European Myeloma Network (EMN) develops guidelines for risk-adapted therapy in myeloma.
7.3. Factors Affecting Prognosis
Factors that can affect prognosis include age, kidney function, cytogenetic abnormalities, and response to initial treatment. The Mayo Stratification for Myeloma and Risk-Adapted Therapy (mSMART) guidelines incorporate these factors to guide treatment decisions.
7.4. Monitoring and Follow-Up
Regular monitoring and follow-up are essential to detect disease progression or relapse. Patients should undergo periodic blood tests, urine tests, and imaging studies. The Leukemia & Lymphoma Society provides resources on monitoring and managing myeloma.
8. What Are Some Common Complications of Myeloma?
Myeloma can lead to various complications, including:
8.1. Bone Damage
Bone damage, including fractures and lytic lesions, is a common complication of myeloma. This can cause pain, disability, and reduced quality of life. The Skeletal Complications Prevention Group (SCPG) develops guidelines for managing bone complications in myeloma.
8.2. Kidney Failure
Kidney failure can occur due to the deposition of myeloma proteins in the kidneys. This can lead to fluid retention, electrolyte imbalances, and the need for dialysis. The Renal Association provides information on kidney disease and myeloma.
8.3. Infections
Infections are a leading cause of morbidity and mortality in myeloma patients. This is due to the immune suppression caused by myeloma and its treatment. The Infectious Diseases Society of America (IDSA) offers guidelines for preventing and treating infections in immunocompromised patients.
8.4. Anemia
Anemia can cause fatigue, weakness, and shortness of breath. It is often treated with blood transfusions or erythropoiesis-stimulating agents (ESAs). The American Society of Hematology (ASH) provides resources on anemia management.
8.5. Hypercalcemia
Hypercalcemia can cause nausea, constipation, confusion, and kidney damage. It is treated with intravenous fluids, bisphosphonates, and other medications. The Endocrine Society offers guidelines for managing hypercalcemia.
8.6. Spinal Cord Compression
Spinal cord compression can occur when myeloma tumors press on the spinal cord. This can cause pain, weakness, and loss of bowel or bladder control. The North American Spine Society (NASS) provides information on spinal cord compression.
9. What Are Some Frequently Asked Questions About Myeloma?
| Question | Answer |
|---|---|
| What is the difference between myeloma and MGUS? | MGUS is a premalignant condition with abnormal plasma cells and M protein, but no symptoms or organ damage. Myeloma is active cancer with symptoms and organ damage. |
| Can myeloma be cured? | While a cure is not always possible, treatments can effectively control the disease and improve quality of life. Stem cell transplantation offers the best chance for long-term remission. |
| What are the latest advances in myeloma treatment? | Recent advances include new targeted therapies, immunotherapies, and CAR T-cell therapy. These treatments have significantly improved survival rates and quality of life for myeloma patients. |
| What is the role of diet and exercise in myeloma management? | A healthy diet and regular exercise can help improve energy levels, boost the immune system, and maintain bone health. Patients should consult with their healthcare team for personalized recommendations. |
| How can I find support for myeloma patients? | Support groups, online forums, and patient advocacy organizations can provide valuable resources and emotional support. The International Myeloma Foundation and the Leukemia & Lymphoma Society offer support programs for myeloma patients and their families. |
| What is the difference between plasmacytoma and multiple myeloma? | Plasmacytoma is a single tumor of plasma cells that can be in the bone (solitary bone plasmacytoma) or in soft tissue (extramedullary plasmacytoma). Multiple myeloma involves multiple tumors throughout the bone marrow and other parts of the body. |
| Are there any clinical trials for myeloma? | Yes, many clinical trials are ongoing to evaluate new treatments for myeloma. Patients may be eligible to participate in clinical trials to access cutting-edge therapies. The National Cancer Institute’s Clinical Trials Search provides a database of clinical trials for myeloma. |
| What are the side effects of myeloma treatment? | Side effects vary depending on the type of treatment but can include fatigue, nausea, hair loss, and increased risk of infection. Healthcare providers can offer strategies to manage side effects and improve quality of life. |
| How is myeloma staged? | Myeloma is staged using the International Staging System (ISS) and Revised International Staging System (R-ISS), which consider factors such as beta-2 microglobulin, albumin, and cytogenetic abnormalities. |
| Can myeloma be prevented? | There is no known way to prevent myeloma, but individuals with risk factors, such as MGUS, should be monitored regularly. Early detection and treatment can improve outcomes. |
10. Where Can You Ask Questions and Get Free Answers?
Dealing with myeloma can be overwhelming, but you’re not alone. Do you have more questions about myeloma disease or other health concerns? Don’t hesitate to ask! At WHAT.EDU.VN, we provide a free platform for you to ask any question and receive answers from knowledgeable experts and community members.
Our mission is to make information accessible and easy to understand. We understand the challenges of finding reliable answers quickly and without cost. That’s why we’ve created a space where you can ask your questions and get the support you need.
Here’s how we can help:
- Free Question Submission: Ask any question you have, no matter how simple or complex.
- Expert Answers: Receive answers from experts and experienced community members.
- Easy-to-Understand Information: Get clear and concise explanations tailored to your needs.
- Community Support: Connect with others who share similar experiences and concerns.
Ready to get started?
Visit WHAT.EDU.VN today and ask your question. Let us help you find the answers you’re looking for, completely free. We are located at 888 Question City Plaza, Seattle, WA 98101, United States. You can also reach us via Whatsapp at +1 (206) 555-7890. Your peace of mind is just a question away.
Don’t wait—ask your question now and take control of your health journey with what.edu.vn.
