What Is Pcos Mean? Polycystic Ovary Syndrome or PCOS is a hormonal disorder common among women of reproductive age, impacting fertility and overall health. At WHAT.EDU.VN, we provide clear answers and guidance to those seeking to understand PCOS, offering insights into its symptoms, causes, and management. Gain knowledge of menstrual irregularities and hormonal imbalances while exploring related conditions like insulin resistance, metabolic syndrome, and infertility.
1. Understanding What Is PCOS Mean: A Comprehensive Guide
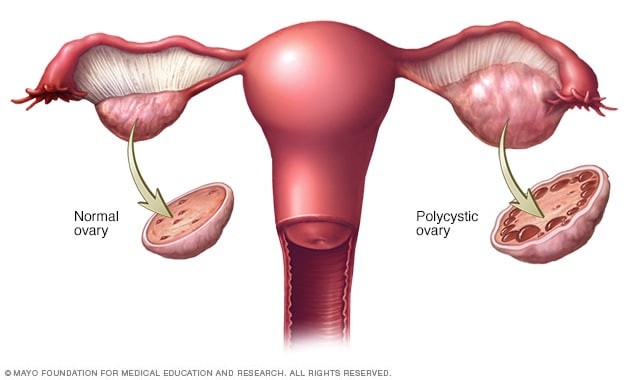
Polycystic Ovary Syndrome (PCOS) is a prevalent hormonal disorder affecting women during their reproductive years. Characterized by irregular menstrual periods, excess androgen levels, and polycystic ovaries, PCOS can significantly impact a woman’s fertility and overall health. The term “polycystic” refers to the presence of multiple small cysts on the ovaries, although not all women with PCOS have these cysts.
PCOS is a complex condition with a wide range of symptoms and potential long-term health risks. Early diagnosis and treatment, along with lifestyle modifications, can help manage the symptoms and reduce the risk of complications. This comprehensive guide will delve into the intricacies of PCOS, exploring its symptoms, causes, diagnosis, treatment options, and potential complications.
1.1. What is the Medical Definition of PCOS?
Medically, PCOS is defined as a syndrome characterized by the presence of at least two of the following three criteria, as defined by the Rotterdam criteria:
- Irregular ovulation: This can manifest as infrequent periods, prolonged periods, or absent periods.
- Clinical or biochemical signs of hyperandrogenism: This refers to elevated levels of androgens, such as testosterone, which can cause symptoms like hirsutism (excess hair growth), acne, and male-pattern baldness.
- Polycystic ovaries on ultrasound: This involves the presence of 12 or more follicles (small sacs containing immature eggs) in each ovary, as visualized on an ultrasound scan.
1.2. What are the Key Features of PCOS?
PCOS is characterized by a combination of hormonal imbalances, irregular periods, and ovarian cysts. Here’s a breakdown of the key features:
- Hormonal Imbalances: Women with PCOS often have elevated levels of androgens, which can disrupt the normal menstrual cycle and lead to various symptoms.
- Irregular Menstrual Periods: This is a hallmark of PCOS, with women experiencing infrequent, irregular, or prolonged periods. Some women may even stop menstruating altogether.
- Polycystic Ovaries: While not always present, the presence of multiple small cysts on the ovaries is a common feature of PCOS. These cysts are actually immature follicles that have failed to release eggs.
1.3. Who is Typically Affected by PCOS?
PCOS primarily affects women of reproductive age, typically starting around the time of their first menstrual period (menarche). However, some women may develop symptoms later in life. The prevalence of PCOS is estimated to be between 6% and 12% of women of reproductive age, making it one of the most common endocrine disorders in this population.
1.4. What is the Impact of PCOS on Overall Health?
PCOS can have a significant impact on a woman’s overall health, both physically and emotionally. Beyond the immediate symptoms of irregular periods and hormonal imbalances, PCOS can increase the risk of several long-term health complications, including:
- Infertility: PCOS is a leading cause of infertility in women, as irregular ovulation can make it difficult to conceive.
- Type 2 Diabetes: Women with PCOS have a higher risk of developing insulin resistance and type 2 diabetes.
- Cardiovascular Disease: PCOS is associated with an increased risk of heart disease, stroke, and other cardiovascular problems.
- Endometrial Cancer: Irregular periods can lead to a thickening of the uterine lining, increasing the risk of endometrial cancer.
- Mental Health Issues: PCOS can contribute to depression, anxiety, and other mental health problems due to the hormonal imbalances and the challenges of managing the condition.
Early diagnosis and management of PCOS are crucial for mitigating these risks and improving a woman’s overall quality of life. If you have questions about PCOS or other health issues, remember that WHAT.EDU.VN is here to provide answers and support.
2. Symptoms of PCOS: Recognizing the Signs
The symptoms of PCOS can vary widely from woman to woman, and some women may experience only mild symptoms, while others may have more severe manifestations. It’s important to be aware of the potential signs of PCOS and to consult a healthcare provider if you suspect you may have the condition.
2.1. Common Signs and Symptoms
Here’s a list of the most common signs and symptoms of PCOS:
- Irregular Periods: Infrequent, irregular, or prolonged menstrual periods are a hallmark of PCOS. Some women may experience fewer than eight periods per year, while others may have periods that last for many days or even weeks.
- Hirsutism: This refers to excessive hair growth on the face, chest, back, or other areas where men typically have hair. Hirsutism is caused by elevated levels of androgens.
- Acne: Severe or persistent acne, particularly on the face, chest, or back, can be a sign of PCOS. Androgens can stimulate the production of sebum, an oily substance that can clog pores and lead to acne.
- Male-Pattern Baldness: Thinning hair or hair loss on the scalp, similar to that seen in men, can occur in women with PCOS due to elevated androgen levels.
- Weight Gain or Difficulty Losing Weight: Many women with PCOS struggle with weight gain or find it difficult to lose weight. Insulin resistance, a common feature of PCOS, can contribute to weight gain.
- Skin Darkening (Acanthosis Nigricans): Dark, velvety patches of skin may develop on the neck, armpits, groin, or under the breasts. This is often a sign of insulin resistance.
 Polycystic ovary syndrome symptoms
Polycystic ovary syndrome symptoms
Alt text: Illustration depicting a healthy ovary versus a polycystic ovary, highlighting the presence of multiple cysts in PCOS.
2.2. Less Common Symptoms
In addition to the more common symptoms, some women with PCOS may experience other, less frequent signs, such as:
- Pelvic Pain: Some women may experience chronic pelvic pain, which can be caused by enlarged ovaries or other factors.
- Anxiety or Depression: Hormonal imbalances and the challenges of managing PCOS can contribute to anxiety and depression.
- Sleep Apnea: This sleep disorder, characterized by pauses in breathing during sleep, is more common in women with PCOS, particularly those who are overweight or obese.
- Infertility: As mentioned earlier, PCOS is a leading cause of infertility in women due to irregular ovulation.
2.3. How Symptoms Vary Among Individuals
The severity and combination of symptoms can vary significantly among women with PCOS. Some women may experience only mild symptoms, such as slightly irregular periods or a few acne breakouts, while others may have more severe symptoms, such as hirsutism, significant weight gain, and difficulty conceiving.
Several factors can influence the severity of symptoms, including:
- Genetics: Family history of PCOS can increase the risk of developing the condition and may influence the severity of symptoms.
- Lifestyle Factors: Diet, exercise, and stress levels can all impact the symptoms of PCOS.
- Underlying Health Conditions: Other health conditions, such as insulin resistance and obesity, can worsen the symptoms of PCOS.
2.4. When to Seek Medical Advice
It’s essential to seek medical advice if you experience any of the following:
- Irregular periods: If your periods are consistently irregular, infrequent, or absent, it’s important to consult a healthcare provider to determine the cause.
- Excessive hair growth: If you notice new or excessive hair growth on your face, chest, back, or other areas, it could be a sign of PCOS or another hormonal disorder.
- Severe acne: Persistent or severe acne that doesn’t respond to over-the-counter treatments may warrant a visit to a dermatologist or healthcare provider.
- Difficulty conceiving: If you’ve been trying to conceive for six months or more without success, it’s important to seek medical advice to evaluate potential causes of infertility.
- Symptoms of insulin resistance: If you experience symptoms such as skin darkening, weight gain, or increased thirst, it could be a sign of insulin resistance, which is often associated with PCOS.
Don’t hesitate to reach out to WHAT.EDU.VN for reliable information and resources to help you understand and manage your health concerns. Our goal is to empower you with the knowledge you need to make informed decisions about your well-being.
3. Exploring the Causes of PCOS
The exact cause of PCOS remains unknown, but it is believed to be a complex interplay of genetic and environmental factors. Several factors have been identified as playing a significant role in the development of PCOS.
3.1. Genetic Predisposition
Research suggests that genetics may play a significant role in the development of PCOS. Women with a family history of PCOS are more likely to develop the condition themselves. Several genes have been identified as potential contributors to PCOS, but more research is needed to fully understand the genetic basis of the disorder.
3.2. Hormonal Imbalances
Hormonal imbalances are a hallmark of PCOS, and they are believed to play a central role in the development of the condition. The key hormonal imbalances associated with PCOS include:
- Elevated Androgen Levels: Women with PCOS often have elevated levels of androgens, such as testosterone and androstenedione. These hormones can contribute to symptoms like hirsutism, acne, and male-pattern baldness.
- Insulin Resistance: Many women with PCOS have insulin resistance, which means that their bodies don’t respond properly to insulin. This can lead to elevated blood sugar levels and an increased risk of type 2 diabetes.
- Luteinizing Hormone (LH) Imbalance: LH is a hormone that stimulates ovulation. In women with PCOS, LH levels may be elevated, which can disrupt the normal menstrual cycle and contribute to irregular ovulation.
3.3. Insulin Resistance and PCOS
Insulin resistance is a common feature of PCOS, and it is believed to play a significant role in the development and progression of the condition. When the body is resistant to insulin, the pancreas produces more insulin to compensate. Elevated insulin levels can then stimulate the ovaries to produce more androgens, exacerbating the hormonal imbalances associated with PCOS.
Insulin resistance can also contribute to weight gain, which can further worsen the symptoms of PCOS. Maintaining a healthy weight and managing insulin resistance are important goals in the management of PCOS.
3.4. The Role of Inflammation
Emerging research suggests that chronic low-grade inflammation may play a role in the development of PCOS. Inflammation can disrupt hormone production and contribute to insulin resistance, both of which are key features of PCOS.
3.5. Lifestyle Factors and Environmental Influences
Lifestyle factors, such as diet, exercise, and stress levels, can also influence the development and severity of PCOS. A diet high in processed foods and sugar can contribute to insulin resistance and inflammation, while regular exercise and stress management techniques can help improve hormone balance and reduce inflammation.
Environmental factors, such as exposure to endocrine-disrupting chemicals, may also play a role in the development of PCOS, but more research is needed in this area.
Understanding the potential causes of PCOS is crucial for developing effective prevention and treatment strategies. While the exact cause of PCOS remains elusive, ongoing research is shedding light on the complex interplay of genetic, hormonal, and environmental factors that contribute to the condition. At WHAT.EDU.VN, we are committed to providing you with the latest information and resources to help you understand and manage your health concerns.
4. Diagnosing PCOS: Identifying the Condition
Diagnosing PCOS can be challenging, as there is no single test that can definitively confirm the diagnosis. Healthcare providers typically rely on a combination of medical history, physical examination, and laboratory tests to diagnose PCOS.
4.1. Diagnostic Criteria
The most widely used diagnostic criteria for PCOS are the Rotterdam criteria, which require the presence of at least two of the following three features:
- Irregular Ovulation: This includes infrequent periods (fewer than eight per year), prolonged periods, or absent periods.
- Clinical or Biochemical Signs of Hyperandrogenism: This refers to symptoms of excess androgens, such as hirsutism, acne, or male-pattern baldness, or elevated androgen levels on blood tests.
- Polycystic Ovaries on Ultrasound: This involves the presence of 12 or more follicles (small sacs containing immature eggs) in each ovary, as visualized on an ultrasound scan.
It’s important to note that not all women with PCOS have polycystic ovaries on ultrasound, and some women with polycystic ovaries do not have PCOS.
4.2. Medical History and Physical Examination
During the initial evaluation, your healthcare provider will ask about your medical history, including your menstrual cycles, symptoms, and family history of PCOS or other hormonal disorders. They will also perform a physical examination to assess for signs of hyperandrogenism, such as hirsutism and acne.
4.3. Blood Tests
Blood tests are an important part of the diagnostic process for PCOS. These tests can help assess hormone levels and identify any underlying medical conditions that may be contributing to your symptoms. Common blood tests for PCOS include:
- Androgen Levels: These tests measure the levels of androgens, such as testosterone and DHEAS, in your blood. Elevated androgen levels are a key feature of PCOS.
- Fasting Glucose and Insulin Levels: These tests help assess insulin resistance. Elevated glucose and insulin levels may indicate insulin resistance.
- Lipid Profile: This test measures cholesterol and triglyceride levels in your blood. Women with PCOS are at increased risk of high cholesterol and triglycerides.
- Thyroid Function Tests: These tests assess thyroid function, as thyroid disorders can sometimes mimic the symptoms of PCOS.
- Prolactin Level: This test measures the level of prolactin, a hormone that can sometimes be elevated in women with PCOS.
4.4. Pelvic Ultrasound
A pelvic ultrasound is often performed to visualize the ovaries and assess for the presence of polycystic ovaries. The ultrasound can also help rule out other potential causes of your symptoms, such as ovarian cysts or tumors.
4.5. Ruling Out Other Conditions
It’s important to rule out other conditions that can mimic the symptoms of PCOS, such as:
- Thyroid Disorders: Both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can cause menstrual irregularities and other symptoms similar to those of PCOS.
- Congenital Adrenal Hyperplasia (CAH): This genetic disorder can cause elevated androgen levels and symptoms similar to those of PCOS.
- Cushing’s Syndrome: This hormonal disorder can cause weight gain, acne, and other symptoms that may resemble those of PCOS.
- Hyperprolactinemia: Elevated prolactin levels can disrupt menstrual cycles and cause symptoms similar to those of PCOS.
A thorough evaluation by a healthcare provider is essential for accurately diagnosing PCOS and ruling out other potential causes of your symptoms. If you have questions or concerns about PCOS or other health issues, don’t hesitate to reach out to WHAT.EDU.VN for reliable information and support.
5. Treatment Options for PCOS: Managing the Condition
While there is no cure for PCOS, there are several effective treatment options available to manage the symptoms and reduce the risk of long-term health complications. Treatment for PCOS is typically tailored to the individual’s specific symptoms and goals.
5.1. Lifestyle Modifications
Lifestyle modifications are often the first-line treatment for PCOS. These include:
- Weight Management: Maintaining a healthy weight is crucial for managing PCOS. Even a modest weight loss of 5-10% can significantly improve hormone balance, menstrual cycles, and fertility.
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean protein can help regulate blood sugar levels, reduce insulin resistance, and promote weight loss.
- Regular Exercise: Regular physical activity can improve insulin sensitivity, promote weight loss, and reduce the risk of cardiovascular disease. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Stress Management: Chronic stress can worsen the symptoms of PCOS. Stress management techniques, such as yoga, meditation, and deep breathing exercises, can help improve hormone balance and reduce stress levels.
5.2. Medications
Several medications are commonly used to treat the symptoms of PCOS:
- Oral Contraceptives: Birth control pills can help regulate menstrual cycles, reduce androgen levels, and improve acne and hirsutism.
- Metformin: This medication is commonly used to treat type 2 diabetes, but it can also be helpful for women with PCOS who have insulin resistance. Metformin can improve insulin sensitivity, regulate menstrual cycles, and promote weight loss.
- Anti-Androgens: These medications, such as spironolactone, can block the effects of androgens and reduce symptoms like hirsutism and acne.
- Fertility Medications: Women with PCOS who are trying to conceive may need fertility medications, such as clomiphene citrate or letrozole, to stimulate ovulation.
5.3. Surgical Options
In some cases, surgery may be an option for women with PCOS who are not responding to other treatments. One surgical procedure that is sometimes used is laparoscopic ovarian drilling, which involves making small holes in the ovaries to reduce androgen production.
5.4. Alternative Therapies
Some women with PCOS may find relief from alternative therapies, such as:
- Acupuncture: Some studies have suggested that acupuncture may help regulate menstrual cycles and improve fertility in women with PCOS.
- Herbal Remedies: Certain herbal remedies, such as saw palmetto and spearmint tea, may help reduce androgen levels and improve symptoms like hirsutism. However, it’s important to talk to your healthcare provider before using any herbal remedies, as they can interact with medications and may not be safe for everyone.
Alt text: Conceptual illustration representing various PCOS treatment options, including lifestyle changes, medication, and alternative therapies.
5.5. Individualized Treatment Plans
The best treatment plan for PCOS is one that is tailored to the individual’s specific symptoms, goals, and medical history. It’s important to work closely with your healthcare provider to develop a treatment plan that is right for you. This may involve a combination of lifestyle modifications, medications, and alternative therapies.
Managing PCOS is an ongoing process, and it’s important to be patient and persistent with your treatment. With the right approach, you can effectively manage your symptoms and reduce your risk of long-term health complications. Remember, WHAT.EDU.VN is here to support you with reliable information and resources to help you navigate your PCOS journey.
6. Potential Complications of PCOS
PCOS can increase the risk of several long-term health complications. Early diagnosis and treatment, along with lifestyle modifications, can help reduce the risk of these complications.
6.1. Infertility
PCOS is a leading cause of infertility in women. Irregular ovulation can make it difficult to conceive, and women with PCOS may need fertility medications or other treatments to help them get pregnant.
6.2. Type 2 Diabetes
Women with PCOS have a higher risk of developing insulin resistance and type 2 diabetes. Maintaining a healthy weight, eating a balanced diet, and getting regular exercise can help reduce the risk of diabetes.
6.3. Cardiovascular Disease
PCOS is associated with an increased risk of heart disease, stroke, and other cardiovascular problems. Managing risk factors such as high cholesterol, high blood pressure, and obesity can help reduce the risk of cardiovascular disease.
6.4. Endometrial Cancer
Irregular periods can lead to a thickening of the uterine lining, increasing the risk of endometrial cancer. Regular screening for endometrial cancer is recommended for women with PCOS who have irregular periods.
6.5. Sleep Apnea
Sleep apnea, a sleep disorder characterized by pauses in breathing during sleep, is more common in women with PCOS, particularly those who are overweight or obese. Sleep apnea can increase the risk of cardiovascular disease and other health problems.
6.6. Mental Health Issues
PCOS can contribute to depression, anxiety, and other mental health problems due to the hormonal imbalances and the challenges of managing the condition. Seeking mental health support, such as therapy or medication, can help improve mental well-being.
6.7. Pregnancy Complications
Women with PCOS are at increased risk of certain pregnancy complications, such as gestational diabetes, preeclampsia (high blood pressure during pregnancy), and premature birth. Careful monitoring during pregnancy is essential to reduce the risk of these complications.
Preventing and managing these potential complications is an important part of PCOS care. Regular check-ups with your healthcare provider, along with lifestyle modifications and appropriate medical treatments, can help you stay healthy and reduce your risk of long-term health problems. At WHAT.EDU.VN, we are dedicated to providing you with the information and resources you need to take control of your health and live your best life with PCOS.
7. Living with PCOS: Tips for Managing Daily Life
Living with PCOS can be challenging, but with the right strategies and support, you can effectively manage your symptoms and improve your quality of life.
7.1. Emotional and Psychological Support
PCOS can have a significant impact on emotional and psychological well-being. It’s important to seek support from friends, family, or a therapist to cope with the emotional challenges of living with PCOS. Support groups can also be a valuable resource for connecting with other women who understand what you’re going through.
7.2. Nutritional Strategies
A healthy diet is crucial for managing PCOS. Focus on eating whole, unprocessed foods, such as fruits, vegetables, whole grains, and lean protein. Limit your intake of processed foods, sugary drinks, and unhealthy fats.
Some specific nutritional strategies that may be helpful for women with PCOS include:
- Eating a low-glycemic index (GI) diet: This can help regulate blood sugar levels and reduce insulin resistance.
- Increasing fiber intake: Fiber can help regulate blood sugar levels and promote weight loss.
- Consuming healthy fats: Healthy fats, such as those found in avocados, nuts, and olive oil, can help improve hormone balance.
- Limiting dairy intake: Some women with PCOS may find that limiting dairy intake improves their symptoms.
7.3. Exercise and Physical Activity
Regular exercise is beneficial for managing PCOS. Aim for at least 150 minutes of moderate-intensity exercise per week. Choose activities that you enjoy, such as walking, running, swimming, or dancing.
7.4. Skincare and Hair Removal Techniques
Managing hirsutism and acne can be challenging. Consider using skincare products that are specifically designed for acne-prone skin. Hair removal techniques, such as waxing, shaving, or laser hair removal, can help manage hirsutism.
7.5. Fertility and Family Planning
If you have PCOS and are trying to conceive, talk to your healthcare provider about fertility treatment options. Fertility medications, such as clomiphene citrate or letrozole, can help stimulate ovulation.
It’s also important to be aware of the potential risks of pregnancy complications in women with PCOS. Careful monitoring during pregnancy is essential to reduce the risk of these complications.
7.6. Long-Term Health Management
PCOS is a chronic condition that requires ongoing management. Regular check-ups with your healthcare provider are essential for monitoring your health and adjusting your treatment plan as needed.
Living with PCOS requires a holistic approach that addresses both the physical and emotional aspects of the condition. By adopting healthy lifestyle habits, seeking support, and working closely with your healthcare provider, you can effectively manage your symptoms and improve your quality of life.
8. Current Research and Future Directions in PCOS
Research on PCOS is ongoing, and scientists are working to better understand the causes of the condition and develop more effective treatments.
8.1. Advances in Understanding PCOS
Recent research has shed light on the complex interplay of genetic, hormonal, and environmental factors that contribute to PCOS. Scientists have identified several genes that may be associated with PCOS, and they are working to understand how these genes interact with environmental factors to increase the risk of developing the condition.
8.2. Emerging Therapies
Several new therapies for PCOS are currently under development. These include:
- New Medications: Researchers are working to develop new medications that can target the underlying hormonal imbalances in PCOS.
- Targeted Therapies: Scientists are exploring targeted therapies that can address specific symptoms of PCOS, such as insulin resistance or hirsutism.
- Lifestyle Interventions: Researchers are investigating the effectiveness of different lifestyle interventions, such as specific dietary patterns or exercise programs, for managing PCOS.
8.3. The Role of Technology in PCOS Management
Technology is playing an increasingly important role in the management of PCOS. Telemedicine, mobile apps, and wearable devices can help women with PCOS track their symptoms, monitor their health, and connect with healthcare providers remotely.
8.4. The Future of PCOS Research
The future of PCOS research is bright. Scientists are making progress in understanding the causes of the condition and developing more effective treatments. With continued research and innovation, we can hope to improve the lives of women with PCOS.
9. Frequently Asked Questions (FAQs) about PCOS
To further clarify common questions and concerns about PCOS, here’s a detailed FAQ section:
| Question | Answer |
|---|---|
| What are the diagnostic criteria for PCOS? | The Rotterdam criteria are most commonly used, requiring at least two of the following: irregular ovulation, clinical or biochemical signs of hyperandrogenism, and polycystic ovaries on ultrasound. |
| Is PCOS a lifelong condition? | Yes, PCOS is a chronic condition, but its symptoms can be managed effectively with lifestyle modifications and medical treatments. |
| Can I get pregnant if I have PCOS? | Yes, many women with PCOS can get pregnant with the help of fertility treatments and lifestyle changes. |
| What is the best diet for PCOS? | A low-glycemic index (GI) diet rich in fruits, vegetables, whole grains, and lean protein is recommended. |
| How does exercise help with PCOS? | Regular exercise can improve insulin sensitivity, promote weight loss, and reduce the risk of cardiovascular disease. |
| What are the potential long-term health risks of PCOS? | Potential risks include infertility, type 2 diabetes, cardiovascular disease, endometrial cancer, sleep apnea, and mental health issues. |
| Are there any natural remedies for PCOS? | Some herbal remedies, such as saw palmetto and spearmint tea, may help reduce androgen levels, but it’s important to talk to your healthcare provider before using them. |
| How often should I see my healthcare provider if I have PCOS? | Regular check-ups with your healthcare provider are essential for monitoring your health and adjusting your treatment plan as needed. The frequency of visits will depend on your individual needs and symptoms. |
| Is there a cure for PCOS? | There is currently no cure for PCOS, but its symptoms can be effectively managed with lifestyle modifications and medical treatments. |
| How does PCOS affect mental health? | PCOS can contribute to depression, anxiety, and other mental health problems due to the hormonal imbalances and the challenges of managing the condition. Seeking mental health support can help improve mental well-being. |
10. Call to Action: Empowering You with Knowledge and Support at WHAT.EDU.VN
Navigating PCOS can be overwhelming, but you don’t have to do it alone. At WHAT.EDU.VN, we’re committed to providing you with the information and support you need to understand and manage your health concerns.
Do you have questions about PCOS, its symptoms, or treatment options? Are you looking for a reliable source of information to help you make informed decisions about your health?
We understand the challenges you face and the importance of having access to accurate and trustworthy information. That’s why we’ve created a platform where you can ask any question and receive prompt, accurate answers from knowledgeable experts.
Visit WHAT.EDU.VN today to ask your questions and receive free answers. Our team of experts is here to provide you with the guidance and support you need to take control of your health.
Contact Us:
- Address: 888 Question City Plaza, Seattle, WA 98101, United States
- WhatsApp: +1 (206) 555-7890
- Website: WHAT.EDU.VN
Don’t hesitate to reach out to us with any questions or concerns you may have. We’re here to help you every step of the way. Take the first step towards better health and well-being by visiting what.edu.vn today!