POTS, or Postural Orthostatic Tachycardia Syndrome, is a condition affecting the autonomic nervous system, leading to a rapid increase in heart rate upon standing. At WHAT.EDU.VN, we aim to provide clear and accessible information to help you understand POTS and its effects, offering solutions and support. Discover more about the intricacies of POTS, orthostatic intolerance, and autonomic dysfunction.
Table of Contents
- What is POTS (Postural Orthostatic Tachycardia Syndrome)?
- What Are the Defining Characteristics of POTS?
- How Is POTS Officially Defined?
- What Symptoms Are Commonly Associated with POTS?
- What is the Impact of POTS on Daily Life?
- How Can Lifestyle Changes Help Manage POTS?
- What Role Does Medication Play in Treating POTS?
- Why Is Early Diagnosis of POTS Important?
- What Is the Autonomic Nervous System and How Does It Relate to POTS?
- How Does the Autonomic Nervous System Function?
- What Is the Role of the Sympathetic Nervous System?
- What Happens in a Healthy Body When Standing Up?
- How Does POTS Affect the Body’s Response to Standing?
- What Causes Postural Orthostatic Tachycardia Syndrome (POTS)?
- Is POTS a Form of Dysautonomia?
- Who Is Most Likely to Develop POTS?
- How Is POTS Diagnosed by Healthcare Professionals?
- What Specific Tests Are Used to Diagnose POTS?
- What Should Patients Do If They Suspect They Have POTS?
- Are There Subtypes or Different Types of POTS?
- How Does Low Blood Volume Affect POTS?
- What Is Neuropathic POTS?
- What Is Hyperadrenergic POTS?
- How Is POTS Treated?
- What Medications Are Commonly Prescribed for POTS?
- What Non-Pharmacological Treatments Are Available for POTS?
- How Does Exercise Help Manage POTS?
- What Dietary Changes Can Help Manage POTS?
- How Important Is Hydration for Managing POTS?
- What Are Some Common POTS Triggers?
- How Can Stress Affect POTS Symptoms?
- Can POTS Affect Mental Health?
- What Mental Health Strategies Can Help POTS Patients?
- How Can POTS Patients Manage Their Symptoms at Home?
- What Assistive Devices Can Help POTS Patients?
- What Is the Long-Term Outlook for People with POTS?
- Can POTS Go Away on Its Own?
- Is POTS a Disability?
- What Resources Are Available for People with POTS?
- How Can Family and Friends Support Someone with POTS?
- What Research Is Being Conducted on POTS?
- Where Can I Ask More Questions About POTS and Get Free Answers?
1. What is POTS (Postural Orthostatic Tachycardia Syndrome)?
Postural Orthostatic Tachycardia Syndrome (POTS) is a condition characterized by an abnormal increase in heart rate upon standing, typically without a significant drop in blood pressure. It’s an autonomic nervous system disorder, impacting involuntary bodily functions. If you’re seeking reliable information and quick answers, turn to WHAT.EDU.VN for free expert insights.
2. What Are the Defining Characteristics of POTS?
The defining characteristics of POTS include a sustained increase in heart rate of 30 beats per minute (bpm) or more within 10 minutes of standing (or 40 bpm in adolescents), often accompanied by symptoms like dizziness, lightheadedness, and fatigue. These symptoms are typically relieved by sitting or lying down.
3. How Is POTS Officially Defined?
Officially, POTS is defined by the diagnostic criteria that include a heart rate increase of at least 30 bpm (40 bpm in those aged 12-19) within 10 minutes of standing, without a significant drop in blood pressure, and the presence of chronic symptoms that worsen upon standing. This definition helps healthcare professionals accurately diagnose the condition.
4. What Symptoms Are Commonly Associated with POTS?
Common symptoms associated with POTS include:
- Dizziness and lightheadedness
- Fainting or near-fainting
- Fatigue
- Brain fog and difficulty concentrating
- Headaches
- Nausea
- Heart palpitations
- Tremors
- Sweating
- Shortness of breath
These symptoms can vary in severity and can significantly impact daily life.
5. What is the Impact of POTS on Daily Life?
The impact of POTS on daily life can be significant, often leading to reduced physical activity, difficulty with work or school, and challenges in maintaining social relationships. The chronic nature of the symptoms can result in a decreased quality of life.
6. How Can Lifestyle Changes Help Manage POTS?
Lifestyle changes can play a crucial role in managing POTS. Recommended strategies include:
- Increasing fluid and salt intake to maintain blood volume
- Wearing compression stockings to improve blood flow
- Avoiding prolonged standing
- Elevating the head of the bed
- Engaging in regular exercise, particularly recumbent exercises like swimming or rowing
These changes help improve blood circulation and reduce symptom severity.
7. What Role Does Medication Play in Treating POTS?
Medication can help manage specific symptoms of POTS. Common medications include:
- Beta-blockers to control heart rate
- Midodrine to increase blood pressure
- Fludrocortisone to help retain sodium and fluids
- Selective serotonin reuptake inhibitors (SSRIs) to improve autonomic function
The choice of medication depends on the individual’s specific symptoms and overall health.
8. Why Is Early Diagnosis of POTS Important?
Early diagnosis of POTS is important because it allows individuals to begin management strategies sooner, potentially preventing the condition from worsening and improving their quality of life. Understanding and addressing POTS early can lead to better symptom control.
9. What Is the Autonomic Nervous System and How Does It Relate to POTS?
The autonomic nervous system (ANS) controls involuntary bodily functions such as heart rate, blood pressure, digestion, and sweating. POTS is a disorder of the ANS, causing it to malfunction and leading to the characteristic symptoms of the syndrome.
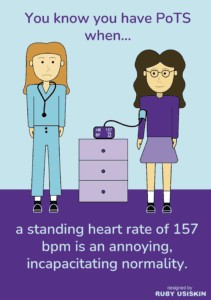 2 females with heart rate monitor
2 females with heart rate monitor
10. How Does the Autonomic Nervous System Function?
The autonomic nervous system functions by regulating bodily processes without conscious effort. It has two main branches: the sympathetic nervous system (which activates the “fight or flight” response) and the parasympathetic nervous system (which promotes “rest and digest” functions). These branches work together to maintain balance in the body.
11. What Is the Role of the Sympathetic Nervous System?
The sympathetic nervous system prepares the body for stress or physical activity by increasing heart rate, blood pressure, and alertness. In POTS, there can be an overactivation of the sympathetic nervous system, leading to excessive heart rate increases and other symptoms.
12. What Happens in a Healthy Body When Standing Up?
In a healthy body, when standing up, blood vessels narrow, and heart rate increases slightly to maintain blood supply to the heart and brain. This ensures that blood pressure remains stable, preventing dizziness or lightheadedness.
13. How Does POTS Affect the Body’s Response to Standing?
In POTS, the automatic adjustments to upright posture do not function correctly. This results in an excessive rise in heart rate, increased norepinephrine in the blood, and altered blood flow to the brain, causing symptoms such as dizziness, fainting, and cognitive impairment.
14. What Causes Postural Orthostatic Tachycardia Syndrome (POTS)?
The exact cause of POTS is not fully understood, but it is believed to involve a combination of factors, including:
- Reduced blood volume
- Autonomic neuropathy (nerve damage)
- Increased levels of norepinephrine
- Autoimmune disorders
- Genetic factors
POTS can also be triggered by events such as viral infections, pregnancy, or surgery.
15. Is POTS a Form of Dysautonomia?
Yes, POTS is a form of dysautonomia, which is a general term for disorders of the autonomic nervous system. Dysautonomia can affect various bodily functions controlled by the ANS, leading to a wide range of symptoms.
16. Who Is Most Likely to Develop POTS?
POTS is more common in women, typically developing between the ages of 15 and 50. Individuals with certain underlying conditions, such as autoimmune disorders, Ehlers-Danlos syndrome, and chronic fatigue syndrome, are also at a higher risk.
17. How Is POTS Diagnosed by Healthcare Professionals?
Healthcare professionals diagnose POTS through a combination of medical history, physical examination, and specific tests. The diagnostic process typically involves:
- Evaluating symptoms and their relationship to posture
- Measuring heart rate and blood pressure while lying down, sitting, and standing
- Performing a tilt table test to assess heart rate and blood pressure changes
A thorough evaluation is necessary to rule out other conditions that may mimic POTS.
18. What Specific Tests Are Used to Diagnose POTS?
Specific tests used to diagnose POTS include:
- Tilt Table Test: Monitors heart rate and blood pressure changes while the patient is tilted from a lying to an upright position.
- Active Stand Test: Involves measuring heart rate and blood pressure after standing for a set period, usually 10 minutes.
- Autonomic Function Testing: Assesses the overall function of the autonomic nervous system.
- Blood Volume Testing: Measures the amount of blood in the body to identify potential deficiencies.
These tests help confirm the diagnosis of POTS and rule out other conditions.
19. What Should Patients Do If They Suspect They Have POTS?
If patients suspect they have POTS, they should:
- Keep a detailed record of their symptoms, including when they occur and what triggers them.
- Consult with a healthcare professional experienced in diagnosing and treating POTS.
- Bring relevant medical history and test results to the appointment.
- Be prepared to describe the impact of their symptoms on daily life.
Seeking timely medical advice can lead to an accurate diagnosis and appropriate management plan.
20. Are There Subtypes or Different Types of POTS?
Yes, there are several subtypes or different types of POTS, including:
- Neuropathic POTS: Caused by damage to the small nerve fibers that control blood vessel constriction.
- Hyperadrenergic POTS: Characterized by excessive levels of norepinephrine, leading to increased heart rate and blood pressure.
- Hypovolemic POTS: Associated with reduced blood volume.
Identifying the specific subtype can help tailor treatment strategies for better outcomes.
21. How Does Low Blood Volume Affect POTS?
Low blood volume can exacerbate POTS symptoms by reducing the amount of blood available to circulate to the brain and other vital organs when standing. This can lead to increased heart rate and other compensatory mechanisms to maintain blood pressure.
22. What Is Neuropathic POTS?
Neuropathic POTS is a subtype characterized by damage to the small nerve fibers that control blood vessel constriction, particularly in the lower extremities. This damage impairs the body’s ability to regulate blood flow, leading to blood pooling and reduced venous return.
23. What Is Hyperadrenergic POTS?
Hyperadrenergic POTS involves excessive levels of norepinephrine, a stress hormone, causing increased heart rate, blood pressure, anxiety, and tremors. This subtype is often associated with a more pronounced “fight or flight” response.
24. How Is POTS Treated?
POTS treatment is aimed at managing symptoms and improving quality of life. Treatment strategies include:
- Lifestyle modifications (increased fluid and salt intake, compression stockings)
- Medications to control heart rate and blood pressure
- Exercise programs to improve cardiovascular fitness
- Stress management techniques
A comprehensive approach is often necessary to address the various aspects of the condition.
25. What Medications Are Commonly Prescribed for POTS?
Commonly prescribed medications for POTS include:
- Beta-blockers (e.g., propranolol): To reduce heart rate
- Midodrine: To increase blood pressure
- Fludrocortisone: To help retain sodium and fluids
- Ivabradine: To specifically lower heart rate without affecting blood pressure
The choice of medication depends on the individual’s specific symptoms and medical history.
26. What Non-Pharmacological Treatments Are Available for POTS?
Non-pharmacological treatments for POTS include:
- Increased Fluid and Salt Intake: To maintain blood volume
- Compression Stockings: To improve blood flow
- Exercise Programs: To enhance cardiovascular fitness
- Dietary Modifications: To manage symptoms
- Stress Management Techniques: To reduce the impact of stress on symptoms
These treatments can be used alone or in combination with medication to manage POTS.
27. How Does Exercise Help Manage POTS?
Exercise helps manage POTS by improving cardiovascular fitness, increasing blood volume, and strengthening muscles that support blood flow. Recumbent exercises like swimming, rowing, and cycling are often recommended to minimize symptoms during exercise.
28. What Dietary Changes Can Help Manage POTS?
Dietary changes that can help manage POTS include:
- Increasing salt intake to help retain fluids
- Eating small, frequent meals to prevent blood sugar fluctuations
- Avoiding processed foods and excessive caffeine
- Ensuring adequate hydration
- Consuming a balanced diet rich in nutrients
These changes can help stabilize blood sugar levels and maintain adequate blood volume.
29. How Important Is Hydration for Managing POTS?
Hydration is crucial for managing POTS because it helps maintain blood volume, which is often reduced in individuals with POTS. Adequate fluid intake can improve blood flow and reduce symptoms like dizziness and lightheadedness.
30. What Are Some Common POTS Triggers?
Common POTS triggers include:
- Prolonged standing
- Dehydration
- Heat exposure
- Stress
- Illness
- Menstrual cycle
Identifying and avoiding these triggers can help minimize symptom flare-ups.
31. How Can Stress Affect POTS Symptoms?
Stress can exacerbate POTS symptoms by activating the sympathetic nervous system, leading to increased heart rate, blood pressure, and anxiety. Managing stress through relaxation techniques can help reduce the severity of POTS symptoms.
32. Can POTS Affect Mental Health?
Yes, POTS can significantly affect mental health. The chronic nature of the condition and its impact on daily life can lead to anxiety, depression, and other mood disorders. Addressing mental health concerns is an important part of comprehensive POTS management.
33. What Mental Health Strategies Can Help POTS Patients?
Mental health strategies that can help POTS patients include:
- Cognitive-behavioral therapy (CBT)
- Mindfulness and meditation
- Relaxation techniques
- Support groups
- Medication, if necessary
These strategies can help individuals cope with the emotional challenges of living with POTS.
34. How Can POTS Patients Manage Their Symptoms at Home?
POTS patients can manage their symptoms at home by:
- Following a structured exercise program
- Maintaining adequate fluid and salt intake
- Wearing compression stockings
- Elevating the head of the bed
- Avoiding prolonged standing
These self-management strategies can help improve overall well-being.
35. What Assistive Devices Can Help POTS Patients?
Assistive devices that can help POTS patients include:
- Compression stockings
- Mobility aids (e.g., canes, walkers)
- Adjustable beds
- Shower chairs
These devices can provide support and improve independence.
36. What Is the Long-Term Outlook for People with POTS?
The long-term outlook for people with POTS varies. Some individuals experience significant improvement in symptoms with treatment and lifestyle modifications, while others continue to struggle with chronic symptoms. Ongoing management and support are essential for maintaining quality of life.
37. Can POTS Go Away on Its Own?
In some cases, POTS can improve or even resolve on its own, particularly if it was triggered by a specific event like a viral infection. However, for many individuals, POTS is a chronic condition that requires ongoing management.
38. Is POTS a Disability?
POTS can be considered a disability if the symptoms significantly impair a person’s ability to perform daily activities and work. The determination of disability status depends on the severity of symptoms and their impact on functioning.
39. What Resources Are Available for People with POTS?
Resources available for people with POTS include:
- POTS support groups and online communities
- Medical professionals specializing in autonomic disorders
- Educational materials and websites
- Disability services and accommodations
These resources can provide valuable information, support, and assistance.
40. How Can Family and Friends Support Someone with POTS?
Family and friends can support someone with POTS by:
- Learning about the condition and its symptoms
- Providing emotional support and understanding
- Assisting with daily tasks and activities
- Encouraging adherence to treatment plans
- Advocating for their needs
Understanding and support can make a significant difference in the life of someone with POTS.
41. What Research Is Being Conducted on POTS?
Research on POTS is ongoing, focusing on:
- Identifying the underlying causes and mechanisms of the condition
- Developing more effective treatments
- Improving diagnostic methods
- Understanding the long-term effects of POTS
These research efforts aim to improve the lives of individuals affected by POTS.
42. Where Can I Ask More Questions About POTS and Get Free Answers?
For more questions about POTS and to receive free answers, visit WHAT.EDU.VN. Our platform offers a wealth of information and expert insights to help you understand and manage POTS effectively.
Do you have more questions about POTS or any other topic? Don’t hesitate to ask on WHAT.EDU.VN and get free, reliable answers from our community of experts. We are located at 888 Question City Plaza, Seattle, WA 98101, United States. You can also reach us on Whatsapp at +1 (206) 555-7890. Visit our website at what.edu.vn for more information.