Polycystic ovaries can be a source of concern and confusion, but WHAT.EDU.VN is here to offer clarity. Polycystic ovary syndrome (PCOS) involves hormonal imbalances and metabolic issues that can affect a woman’s overall health and well-being, especially menstrual cycles. Understanding PCOS is the first step toward managing it effectively. You’ll gain actionable insights and explore potential avenues for seeking professional help and discover ways to find fast and free answers on WHAT.EDU.VN. Let’s dive into understanding the symptoms, diagnostic criteria, and long-term health implications of polycystic ovaries.
1. Understanding Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome (PCOS) is a prevalent hormonal disorder affecting women of reproductive age. It is characterized by infrequent or prolonged menstrual periods, excess androgen levels, and/or polycystic ovaries. This syndrome is not merely a reproductive issue; it has far-reaching implications for overall health, impacting metabolism, cardiovascular health, and psychological well-being. Understanding the complexities of PCOS is crucial for effective management and improving the quality of life for those affected.
1.1. Definition and Key Features
PCOS is defined by a combination of hormonal and metabolic imbalances. The key features include:
- Irregular Menstrual Cycles: Oligomenorrhea (infrequent periods) or amenorrhea (absence of periods).
- Hyperandrogenism: Elevated levels of androgens (male hormones), leading to symptoms like hirsutism (excess hair growth), acne, and male-pattern baldness.
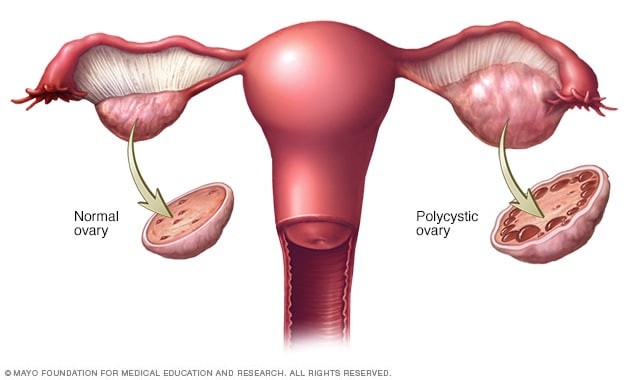
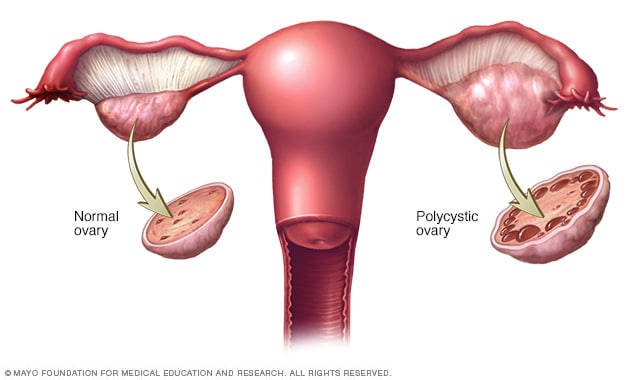
- Polycystic Ovaries: The presence of multiple small follicles (cysts) on the ovaries, detectable through ultrasound.
1.2. Prevalence and Impact
PCOS affects approximately 6-12% of women of reproductive age worldwide, making it one of the most common endocrine disorders in this population. Its impact extends beyond reproductive health, increasing the risk of several long-term complications:
- Infertility: Irregular ovulation is a primary cause of infertility in women with PCOS.
- Metabolic Syndrome: Increased risk of insulin resistance, type 2 diabetes, high blood pressure, and cardiovascular disease.
- Mental Health Disorders: Higher rates of depression, anxiety, and eating disorders.
- Endometrial Cancer: Increased risk due to prolonged exposure to estrogen without regular shedding of the uterine lining.
1.3. Diagnostic Criteria (Rotterdam Criteria)
The Rotterdam criteria, established in 2003, are the most widely used for diagnosing PCOS. A diagnosis requires the presence of at least two of the following three criteria:
- Oligo-ovulation or Anovulation: Irregular, infrequent, or absent menstrual cycles.
- Clinical and/or Biochemical Signs of Hyperandrogenism:
- Clinical: Hirsutism (excess hair growth), acne, or male-pattern baldness.
- Biochemical: Elevated levels of androgens (e.g., testosterone) in the blood.
- Polycystic Ovaries on Ultrasound: The presence of 12 or more follicles measuring 2-9 mm in diameter, and/or increased ovarian volume (>10 mL) in at least one ovary.
It’s important to note that other conditions that can mimic PCOS (such as thyroid disorders, congenital adrenal hyperplasia, and androgen-secreting tumors) must be excluded before a PCOS diagnosis is confirmed.
2. Symptoms of Polycystic Ovaries
The symptoms of PCOS can vary widely among individuals. Some women experience mild symptoms, while others have more severe manifestations. Common symptoms include menstrual irregularities, signs of hyperandrogenism, and polycystic ovaries detected on ultrasound.
2.1. Menstrual Irregularities
Menstrual irregularities are a hallmark of PCOS and can manifest in various ways:
- Oligomenorrhea: Infrequent menstrual periods (fewer than eight periods per year).
- Amenorrhea: Absence of menstrual periods for three months or longer.
- Irregular Cycles: Cycles that vary significantly in length (e.g., some cycles are 25 days, while others are 45 days).
- Heavy Bleeding: In some cases, when a period does occur, it may be abnormally heavy or prolonged.
These irregularities are primarily due to hormonal imbalances that disrupt normal ovulation.
2.2. Signs of Hyperandrogenism
Excess androgens can lead to several noticeable symptoms:
- Hirsutism: Excess hair growth on the face, chest, back, or abdomen. This is one of the most common and distressing symptoms for women with PCOS.
- Acne: Persistent or severe acne, often resistant to typical treatments.
- Male-Pattern Baldness: Thinning hair on the scalp, particularly around the hairline.
- Voice Deepening: Although less common, some women may experience a deepening of the voice.
- Increased Muscle Mass: In rare cases, women may notice an increase in muscle mass.
The severity of these symptoms can vary based on individual sensitivity to androgens.
2.3. Polycystic Ovaries on Ultrasound
Polycystic ovaries are characterized by the presence of multiple small follicles (cysts) on the ovaries. On ultrasound, these appear as a “string of pearls” around the edge of the ovary.
It’s important to note:
- Not all women with PCOS have polycystic ovaries: Some women may have normal-appearing ovaries on ultrasound but still meet other diagnostic criteria for PCOS.
- Polycystic ovaries can occur without PCOS: Some women without PCOS may have polycystic ovaries, highlighting the importance of considering all diagnostic criteria.
2.4. Other Common Symptoms
Besides the primary symptoms, women with PCOS may experience:
- Weight Gain or Difficulty Losing Weight: Insulin resistance can lead to weight gain, especially around the abdomen, and make it challenging to lose weight.
- Skin Darkening: Patches of dark, velvety skin (acanthosis nigricans) may appear on the neck, armpits, or groin, indicating insulin resistance.
- Fatigue: Persistent fatigue can be a significant issue for some women with PCOS.
- Mood Changes: Increased risk of depression, anxiety, and mood swings.
- Sleep Apnea: Disrupted sleep patterns due to pauses in breathing during sleep.
- Infertility: Difficulty conceiving due to irregular or absent ovulation.
2.5. Symptom Variability
The presentation of PCOS can vary considerably among individuals. Some women may primarily experience menstrual irregularities, while others are more troubled by hyperandrogenic symptoms. The reasons for this variability are not fully understood, but genetic and environmental factors are believed to play a role.
3. Causes and Risk Factors of Polycystic Ovary Syndrome
The exact cause of PCOS is not fully understood, but it is believed to be a complex interplay of genetic and environmental factors. Several key factors contribute to the development of PCOS.
3.1. Genetic Factors
Genetic predisposition plays a significant role in the development of PCOS. Women with a family history of PCOS are more likely to develop the condition themselves.
- Family History: Having a mother, sister, or aunt with PCOS increases the risk.
- Gene Studies: Research has identified several genes that may be associated with PCOS, though no single gene is definitively responsible.
3.2. Insulin Resistance
Insulin resistance is a common feature of PCOS, where the body’s cells do not respond effectively to insulin. This leads to elevated levels of insulin in the blood, which can have several adverse effects.
- Increased Androgen Production: High insulin levels stimulate the ovaries to produce more androgens, contributing to hyperandrogenism.
- Weight Gain: Insulin resistance can lead to weight gain, particularly around the abdomen, which further exacerbates insulin resistance.
- Impaired Glucose Metabolism: Over time, insulin resistance can lead to impaired glucose tolerance and an increased risk of type 2 diabetes.
3.3. Hormonal Imbalances
Hormonal imbalances are central to PCOS, affecting the menstrual cycle and ovulation.
- Elevated Androgens: High levels of androgens (such as testosterone) disrupt the normal development of follicles in the ovaries, leading to polycystic ovaries and irregular ovulation.
- Luteinizing Hormone (LH) Imbalance: Some women with PCOS have elevated levels of LH, which can also contribute to increased androgen production.
- Follicle-Stimulating Hormone (FSH) Imbalance: The ratio of LH to FSH may be altered, affecting normal follicular development.
3.4. Chronic Low-Grade Inflammation
Emerging research suggests that chronic low-grade inflammation may play a role in PCOS.
- Inflammatory Markers: Women with PCOS often have elevated levels of inflammatory markers in their blood, such as C-reactive protein (CRP) and interleukin-6 (IL-6).
- Impact on Ovaries: Inflammation may contribute to increased androgen production and impaired ovarian function.
3.5. Environmental Factors
Environmental factors, such as diet and lifestyle, can also influence the development and severity of PCOS.
- Diet: High intake of processed foods, sugary beverages, and unhealthy fats can exacerbate insulin resistance and inflammation.
- Lack of Physical Activity: Sedentary lifestyles contribute to insulin resistance and weight gain.
- Exposure to Endocrine Disruptors: Certain chemicals in the environment (such as bisphenol A (BPA) and phthalates) may disrupt hormone function and contribute to PCOS.
3.6. Risk Factors
Several risk factors increase the likelihood of developing PCOS:
- Family History: As mentioned earlier, having a family history of PCOS is a significant risk factor.
- Obesity: Being overweight or obese increases the risk of insulin resistance and PCOS.
- Insulin Resistance: Individuals with pre-existing insulin resistance are at higher risk.
- Ethnicity: Certain ethnic groups (such as Hispanic and African American women) may have a higher prevalence of PCOS.
4. Diagnosis of Polycystic Ovary Syndrome
Diagnosing PCOS involves a combination of medical history, physical examination, and diagnostic tests. The Rotterdam criteria are widely used to establish a diagnosis.
4.1. Medical History and Physical Examination
The diagnostic process typically begins with a detailed medical history and physical examination.
- Medical History: The healthcare provider will ask about menstrual cycles, symptoms of hyperandrogenism, weight history, and family history of PCOS or related conditions.
- Physical Examination: The examination may include assessing for signs of hirsutism, acne, and acanthosis nigricans. Blood pressure and BMI (body mass index) are also usually checked.
4.2. Blood Tests
Blood tests are essential for assessing hormone levels and ruling out other conditions.
- Hormone Levels:
- Testosterone: Elevated levels can indicate hyperandrogenism.
- Free Androgen Index (FAI): Measures the amount of testosterone that is not bound to proteins in the blood, providing a more accurate assessment of androgen activity.
- Dehydroepiandrosterone Sulfate (DHEAS): Elevated levels can indicate adrenal gland involvement in androgen production.
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH): Assessing the ratio of LH to FSH can provide insights into hormonal imbalances.
- Estradiol: Measures estrogen levels.
- Prolactin: Elevated levels can indicate other conditions that mimic PCOS.
- Glucose and Insulin Levels:
- Fasting Glucose: Measures blood sugar levels after fasting to assess for insulin resistance.
- Oral Glucose Tolerance Test (OGTT): Measures blood sugar levels over a period of two hours after consuming a sugary drink to assess how the body processes glucose.
- Fasting Insulin: Measures insulin levels after fasting to assess for insulin resistance.
- Lipid Profile:
- Cholesterol and Triglycerides: Assesses for abnormal lipid levels, which are common in women with PCOS.
- Thyroid Function Tests:
- Thyroid-Stimulating Hormone (TSH): Rules out thyroid disorders that can cause menstrual irregularities.
4.3. Pelvic Ultrasound
A pelvic ultrasound is used to visualize the ovaries and assess for polycystic ovaries.
- Transvaginal Ultrasound: A probe is inserted into the vagina to provide a clearer image of the ovaries.
- Findings: The presence of 12 or more follicles measuring 2-9 mm in diameter, and/or increased ovarian volume (>10 mL) in at least one ovary, indicates polycystic ovaries.
4.4. Ruling Out Other Conditions
It is crucial to rule out other conditions that can mimic PCOS, such as:
- Thyroid Disorders: Hyperthyroidism or hypothyroidism.
- Congenital Adrenal Hyperplasia (CAH): A genetic disorder affecting the adrenal glands.
- Androgen-Secreting Tumors: Tumors in the ovaries or adrenal glands that produce androgens.
- Hyperprolactinemia: Elevated levels of prolactin.
4.5. Diagnostic Challenges
Diagnosing PCOS can be challenging due to the variability in symptoms and the lack of a single definitive test. It is essential to consider all clinical, biochemical, and ultrasound findings to make an accurate diagnosis.
5. Health Implications and Complications of Polycystic Ovaries
PCOS is associated with several short-term and long-term health implications. Managing these complications is a key aspect of PCOS care.
5.1. Reproductive Health
PCOS significantly affects reproductive health:
- Infertility: Irregular ovulation is a primary cause of infertility in women with PCOS.
- Pregnancy Complications: Increased risk of gestational diabetes, preeclampsia (high blood pressure during pregnancy), and preterm birth.
- Miscarriage: Higher rates of miscarriage in early pregnancy.
5.2. Metabolic Health
PCOS increases the risk of metabolic disorders:
- Insulin Resistance: A common feature of PCOS, leading to elevated insulin levels and an increased risk of type 2 diabetes.
- Type 2 Diabetes: Women with PCOS have a significantly higher risk of developing type 2 diabetes.
- Metabolic Syndrome: A cluster of conditions including high blood pressure, high blood sugar, abnormal cholesterol levels, and excess abdominal fat, increasing the risk of cardiovascular disease.
5.3. Cardiovascular Health
PCOS is associated with an increased risk of cardiovascular disease:
- High Blood Pressure: Common in women with PCOS, contributing to cardiovascular risk.
- Abnormal Cholesterol Levels: Higher levels of LDL (bad) cholesterol and lower levels of HDL (good) cholesterol.
- Increased Risk of Heart Disease: Over time, metabolic and hormonal imbalances can lead to an increased risk of heart attack and stroke.
5.4. Mental Health
PCOS can affect mental health:
- Depression and Anxiety: Women with PCOS have higher rates of depression and anxiety.
- Body Image Issues: Symptoms like hirsutism and acne can lead to body image concerns and low self-esteem.
- Eating Disorders: Increased risk of eating disorders, such as binge eating and bulimia.
5.5. Endometrial Cancer
PCOS increases the risk of endometrial cancer:
- Prolonged Estrogen Exposure: Irregular or absent periods lead to prolonged exposure of the uterine lining to estrogen without regular shedding, increasing the risk of endometrial hyperplasia (thickening of the uterine lining) and cancer.
5.6. Sleep Apnea
PCOS is associated with sleep apnea:
- Obstructive Sleep Apnea: Pauses in breathing during sleep, leading to disrupted sleep patterns and increased risk of cardiovascular and metabolic complications.
5.7. Non-Alcoholic Fatty Liver Disease (NAFLD)
PCOS increases the risk of NAFLD:
- Fat Accumulation in the Liver: NAFLD is characterized by the accumulation of fat in the liver, which can lead to liver inflammation and damage.
5.8. Long-Term Health Risks
The long-term health risks associated with PCOS include:
- Increased Risk of Chronic Diseases: Higher rates of diabetes, cardiovascular disease, and certain types of cancer.
- Reduced Quality of Life: Due to the physical and psychological impact of PCOS symptoms and complications.
6. Managing Polycystic Ovary Syndrome
Managing PCOS involves a combination of lifestyle modifications, medical treatments, and supportive therapies. The goals of management are to alleviate symptoms, reduce the risk of complications, and improve quality of life.
6.1. Lifestyle Modifications
Lifestyle modifications are often the first line of treatment for PCOS:
- Weight Management:
- Diet: A balanced diet that is low in processed foods, sugary beverages, and unhealthy fats. Focus on whole foods, lean proteins, and complex carbohydrates.
- Exercise: Regular physical activity, including both aerobic exercise and strength training, can improve insulin sensitivity and promote weight loss. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Dietary Changes:
- Low Glycemic Index (GI) Diet: Choosing foods with a low GI can help stabilize blood sugar levels and improve insulin sensitivity.
- Increased Fiber Intake: Fiber helps regulate blood sugar levels and promotes satiety.
- Healthy Fats: Incorporating healthy fats, such as those found in avocados, nuts, and olive oil, can improve insulin sensitivity and reduce inflammation.
- Regular Exercise:
- Aerobic Exercise: Activities like walking, running, cycling, and swimming can improve cardiovascular health and insulin sensitivity.
- Strength Training: Building muscle mass can increase metabolism and improve insulin sensitivity.
6.2. Medical Treatments
Medical treatments can help manage specific symptoms and reduce the risk of complications:
- Hormonal Birth Control:
- Oral Contraceptive Pills (OCPs): Regulate menstrual cycles, reduce androgen levels, and decrease the risk of endometrial cancer.
- Hormonal IUDs: Can help regulate menstrual bleeding and reduce the risk of endometrial hyperplasia.
- Anti-Androgen Medications:
- Spironolactone: Blocks the effects of androgens, reducing hirsutism and acne.
- Finasteride: Another anti-androgen medication that can reduce hirsutism and male-pattern baldness.
- Insulin-Sensitizing Medications:
- Metformin: Improves insulin sensitivity, reduces blood sugar levels, and can help regulate menstrual cycles.
- Inositol: A natural supplement that can improve insulin sensitivity and ovarian function.
- Fertility Treatments:
- Clomiphene Citrate: An oral medication that stimulates ovulation.
- Letrozole: Another oral medication that can stimulate ovulation, often used as a first-line treatment for infertility in women with PCOS.
- Gonadotropins: Injectable medications that stimulate ovulation.
- In Vitro Fertilization (IVF): A more advanced fertility treatment that involves retrieving eggs from the ovaries, fertilizing them in a lab, and transferring the resulting embryos to the uterus.
6.3. Symptom-Specific Treatments
Specific treatments can target individual symptoms:
- Hirsutism:
- Shaving, Waxing, and Laser Hair Removal: Methods for removing unwanted hair.
- Eflornithine Cream: A topical cream that can slow hair growth.
- Acne:
- Topical Treatments: Benzoyl peroxide, salicylic acid, and retinoids.
- Oral Antibiotics: For more severe acne.
- Isotretinoin: A powerful medication for severe, treatment-resistant acne.
- Mental Health Support:
- Therapy: Cognitive-behavioral therapy (CBT) and other forms of therapy can help manage depression, anxiety, and body image issues.
- Medications: Antidepressants and anti-anxiety medications may be prescribed.
6.4. Monitoring and Prevention
Regular monitoring and preventive measures are crucial for managing long-term health risks:
- Regular Check-Ups: Monitoring blood pressure, cholesterol levels, and blood sugar levels.
- Screening for Complications: Screening for diabetes, cardiovascular disease, and endometrial cancer.
- Lifestyle Management: Maintaining a healthy lifestyle to reduce the risk of complications.
6.5. Complementary and Alternative Therapies
Some women find complementary and alternative therapies helpful in managing PCOS:
- Acupuncture: May help regulate menstrual cycles and reduce stress.
- Herbal Supplements: Some herbal supplements, such as spearmint tea, may help reduce androgen levels.
- Mind-Body Practices: Yoga, meditation, and mindfulness can help reduce stress and improve overall well-being.
Disclaimer: It is essential to consult with a healthcare provider before starting any new treatment, including complementary and alternative therapies.
7. Seeking Help and Support for Polycystic Ovaries
Navigating life with PCOS can be challenging, but there are many resources available to help you manage the condition and improve your quality of life.
7.1. When to See a Doctor
It is important to see a doctor if you experience:
- Irregular or Absent Periods: If your menstrual cycles are irregular or if you have missed periods for three months or longer.
- Symptoms of Hyperandrogenism: Such as hirsutism, acne, or male-pattern baldness.
- Difficulty Conceiving: If you have been trying to conceive for six months or longer without success.
- Symptoms of Depression or Anxiety: If you are feeling persistently sad, anxious, or overwhelmed.
- Signs of Insulin Resistance: Such as acanthosis nigricans or frequent infections.
7.2. Finding a Healthcare Provider
Several types of healthcare providers can help manage PCOS:
- Primary Care Physician (PCP): Can provide initial evaluation and refer you to specialists.
- Gynecologist: Specializes in women’s reproductive health and can diagnose and treat PCOS.
- Endocrinologist: Specializes in hormonal disorders and can provide comprehensive management of PCOS.
- Reproductive Endocrinologist: Specializes in infertility and can help women with PCOS who are trying to conceive.
- Dermatologist: Can help manage skin-related symptoms like acne and hirsutism.
- Mental Health Professional: Can provide therapy and support for mental health issues.
7.3. Questions to Ask Your Doctor
When you see your doctor, it can be helpful to ask specific questions:
- “What are the treatment options for my specific symptoms?”
- “What lifestyle changes can I make to improve my PCOS?”
- “What are the potential side effects of the recommended treatments?”
- “How often should I have follow-up appointments?”
- “Are there any support groups or resources you recommend?”
7.4. Support Groups and Online Communities
Joining a support group or online community can provide valuable emotional support and information:
- PCOS Awareness Association: Offers resources, support groups, and educational materials.
- The PCOS Challenge: Provides online forums, webinars, and educational programs.
- Verity PCOS: A UK-based organization offering support and information for women with PCOS.
7.5. Managing the Emotional Impact of PCOS
PCOS can have a significant impact on emotional well-being. Strategies for managing the emotional impact include:
- Seeking Therapy: Cognitive-behavioral therapy (CBT) can help manage depression, anxiety, and body image issues.
- Practicing Self-Care: Engaging in activities that promote relaxation and well-being, such as yoga, meditation, and spending time in nature.
- Building a Support Network: Connecting with friends, family, and other women with PCOS for emotional support.
- Setting Realistic Goals: Focusing on achievable goals and celebrating small victories.
7.6. Resources for Further Information
Numerous resources provide accurate and up-to-date information about PCOS:
- The Office on Women’s Health (OASH): Offers comprehensive information about PCOS.
- The American College of Obstetricians and Gynecologists (ACOG): Provides guidelines and resources for healthcare providers and patients.
- The National Institutes of Health (NIH): Conducts research on PCOS and provides information for the public.
8. FAQs About Polycystic Ovaries
Here are some frequently asked questions about polycystic ovaries and PCOS:
| Question | Answer |
|---|---|
| What exactly are polycystic ovaries? | Polycystic ovaries are characterized by the presence of multiple small follicles (cysts) on the ovaries, detectable through ultrasound. Not all women with PCOS have polycystic ovaries, and some women without PCOS may have polycystic ovaries. |
| How is PCOS diagnosed? | PCOS is diagnosed based on the Rotterdam criteria, which include irregular or absent periods, signs of hyperandrogenism (clinical or biochemical), and polycystic ovaries on ultrasound. At least two of these three criteria must be present for a diagnosis, and other conditions must be ruled out. |
| Can PCOS be cured? | There is no cure for PCOS, but it can be effectively managed with lifestyle modifications, medical treatments, and supportive therapies. The goals of management are to alleviate symptoms, reduce the risk of complications, and improve quality of life. |
| How does PCOS affect fertility? | PCOS can cause infertility due to irregular or absent ovulation. Hormonal imbalances disrupt the normal development of follicles in the ovaries, making it difficult to conceive. Fertility treatments, such as clomiphene citrate, letrozole, and IVF, can help women with PCOS conceive. |
| What are the long-term health risks associated with PCOS? | PCOS is associated with several long-term health risks, including an increased risk of type 2 diabetes, cardiovascular disease, metabolic syndrome, endometrial cancer, and sleep apnea. Regular monitoring and preventive measures are crucial for managing these risks. |
| What lifestyle changes can help manage PCOS? | Lifestyle modifications, such as weight management, dietary changes, and regular exercise, can significantly improve PCOS. A balanced diet that is low in processed foods and sugary beverages, along with regular physical activity, can improve insulin sensitivity and promote weight loss. |
| What medications are used to treat PCOS? | Medications used to treat PCOS include hormonal birth control pills (OCPs), anti-androgen medications (such as spironolactone), and insulin-sensitizing medications (such as metformin). OCPs can regulate menstrual cycles and reduce androgen levels, while anti-androgens can reduce hirsutism and acne. Metformin improves insulin sensitivity and can help regulate menstrual cycles. |
| How does insulin resistance relate to PCOS? | Insulin resistance is a common feature of PCOS, where the body’s cells do not respond effectively to insulin. This leads to elevated levels of insulin in the blood, which can stimulate the ovaries to produce more androgens, contributing to hyperandrogenism and irregular ovulation. |
| Can PCOS affect mental health? | Yes, PCOS can affect mental health. Women with PCOS have higher rates of depression, anxiety, and body image issues. Seeking therapy, practicing self-care, and building a support network can help manage the emotional impact of PCOS. |
| What is the role of genetics in PCOS? | Genetic predisposition plays a significant role in the development of PCOS. Women with a family history of PCOS are more likely to develop the condition themselves. Research has identified several genes that may be associated with PCOS, though no single gene is definitively responsible. |

9. The Importance of Early Detection and Intervention
Early detection and intervention are crucial for managing PCOS and reducing the risk of long-term complications. Recognizing the symptoms of PCOS and seeking timely medical care can lead to earlier diagnosis and more effective management.
9.1. Benefits of Early Diagnosis
Early diagnosis of PCOS offers several benefits:
- Improved Symptom Management: Early treatment can help alleviate symptoms like irregular periods, hirsutism, and acne.
- Reduced Risk of Complications: Early intervention can reduce the risk of developing long-term complications like type 2 diabetes, cardiovascular disease, and endometrial cancer.
- Improved Fertility Outcomes: Early fertility treatments can increase the chances of conceiving.
- Enhanced Quality of Life: Effective management of PCOS can improve overall quality of life and emotional well-being.
9.2. Steps to Take if You Suspect You Have PCOS
If you suspect you have PCOS, take the following steps:
- Consult a Healthcare Provider: Schedule an appointment with your primary care physician, gynecologist, or endocrinologist for evaluation.
- Provide a Detailed Medical History: Share information about your menstrual cycles, symptoms, and family history.
- Undergo Diagnostic Testing: Participate in blood tests and a pelvic ultrasound as recommended by your healthcare provider.
- Follow Treatment Recommendations: Adhere to the treatment plan developed by your healthcare provider, which may include lifestyle modifications and medications.
- Attend Follow-Up Appointments: Regularly attend follow-up appointments to monitor your condition and adjust your treatment plan as needed.
9.3. Support and Resources at WHAT.EDU.VN
At WHAT.EDU.VN, we understand the challenges of living with PCOS. We offer a platform where you can ask any question and receive free answers from knowledgeable individuals. If you’re struggling with PCOS or suspect you might have it, don’t hesitate to reach out. Our community is here to support you with accurate information and compassionate guidance.
We encourage you to visit WHAT.EDU.VN and ask your questions today. Our team is dedicated to providing the answers you need to manage PCOS effectively and improve your overall well-being.
Contact Information:
- Address: 888 Question City Plaza, Seattle, WA 98101, United States
- WhatsApp: +1 (206) 555-7890
- Website: WHAT.EDU.VN
Remember, you’re not alone in this journey. Let what.edu.vn be your partner in understanding and managing polycystic ovaries.